Every pregnant woman wants a positive birth experience. Every member of staff working in a maternity service wants to provide safe, high-quality care.
In most cases, that’s what happens. But when things go wrong, the consequences for mothers, babies, their families – and staff – can be devastating.
In 2017, CQC reported on the findings of our first round of comprehensive inspections of all NHS acute hospital services in England. Our report highlighted concerns about the safety of maternity services, with half of all maternity services rated as requires improvement or inadequate for the key question ‘are maternity services safe?’.
It also highlighted concerns about the impact of increasing numbers of women with complex pregnancies and the national shortage of midwives and obstetricians. In addition, we raised concerns about the culture and leadership of some maternity services and revealed evidence of poor multidisciplinary team working and a failure to review and learn from adverse events in the maternity services of some hospitals.
Our current NHS maternity service ratings show some improvement since our first round of comprehensive inspections, and the number of services rated inadequate for safety has reduced considerably. While almost 61% of maternity services are rated good for safety and 1% are outstanding, just under 38% are still rated requires improvement for safety (figure 1). For these services, improvements focused on developing their safety culture are required to narrow the variation that still exists and ensure that all women have access to high-quality maternity care.
Figure 1
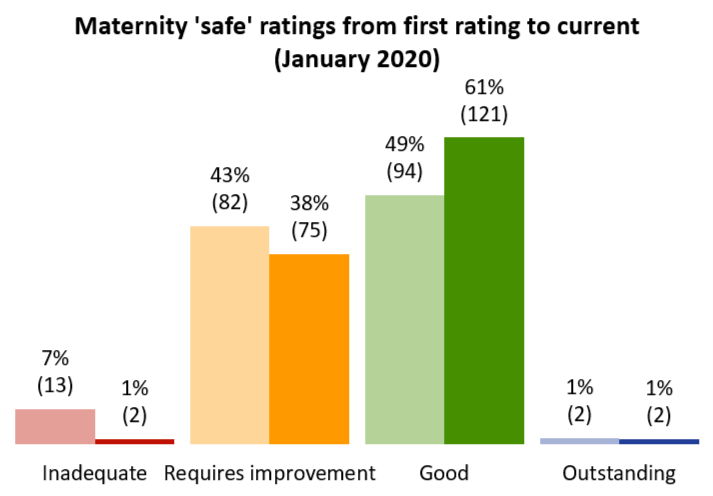
Source: CQC ratings data, all first ratings, and snapshot at 20 January 2020
Maternity services stand out as one of the core services we inspect that is not making improvements in safety fast enough. It is particularly concerning that in some of our inspections where services have been rated inadequate or requires improvement, we have found that the issues identified in the 2015 Kirkup report – staff not having the right skills or knowledge; poor working relationships between obstetricians, midwives and neonatologists; poor risk assessments; and failures to ensure that there is an investigation and learning from when things go wrong – are still affecting the safety of maternity care today.
When looked at internationally, perinatal mortality rates in the UK remain higher than many other European peers and other similar high-income countries. The 2019 MBRRACE-UK reports made it clear that in order to achieve the national ambition to halve the perinatal mortality rate in England by 2025 a greater rate of decline in the national rate will be required than has been seen over recent years. The reports also noted that while most women are getting good care, factors including ethnicity increased risk significantly, with black women five times more likely to die as a result of complications in their pregnancy than white women. Neonatal mortality is also considerably higher for babies of black or Asian ethnicity.
In our report on patient safety, Opening the Door to Change, we called for a radical transformation in the safety culture of the NHS. Nowhere is this more important than in maternity services where high-risk events may be uncommon – 9.2 maternal deaths per 100,000 pregnancies in the UK, and 3.7 stillbirths and 1.7 neonatal deaths per 1,000 births in England MBRRACE-UK reports – but if they are poorly managed, can lead to devastating outcomes for mothers and their babies.
In common with all health and care staff, staff working in maternity services want to provide the best care possible. But there are some consistent issues that affect their ability to provide this care.
This briefing is intended to help maternity services, their trust boards and stakeholders to focus on where they need to improve to ensure that women and babies get consistently good, safe care.
It focuses on three key areas for improvement and is based on:
- analysis of a sample of current CQC inspection reports for services that have been rated as outstanding or inadequate
- the findings from the 2019 CQC maternity survey
- discussion with providers and members of the public at a CQC NHS co-production workshop held in February 2019
Governance, leadership and risk management
Board and leadership teams have a key role to play in making sure that maternity services have staff with the required knowledge and skills, and who work effectively as multidisciplinary teams, so that they are able to recognise and act on any changes that move a pregnancy from low-risk to high-risk.
This includes responding effectively to emergency situations and/or when a patient’s condition is deteriorating. To achieve this, leaders need to ensure that there are strong assurance and risk management processes in place. Leaders at service level also need to be accessible and to promote an inclusive culture in which staff feel able to raise concerns and make suggestions for improvement.
Good leadership is an important element in driving improvement in quality and safety. In our analysis of maternity services, the ratings for safe and well-led were the same in 61% of services, which was the closest alignment between safe and any of the other key questions.
Services that were rated as outstanding had clear governance processes in place with effective policies, assurance, risk management and leadership at every level. These approaches were seen to encourage openness and continuous learning, with effective incident reporting and investigations, and learning processes in place. Services that prioritised learning were able to ensure that staff had the correct skills, knowledge and experience to do their job, and that they were supported to maintain and further develop their professional skills and experience.
In contrast, where services were lacking clear governance and leadership structures, there was evidence that leadership teams were not effectively monitoring failures in teamworking, core staff training competencies and managing serious incident investigations – posing obvious risks to patient care.
The Government’s action plan Safer maternity care: Next steps towards the national maternity ambition set out plans to introduce a board-level maternity safety champion to ensure that there is a board-level focus on improving safety and outcomes in maternity. We welcome the introduction of these safety champions, the publication of guidance for maternity safety champions by NHS England and NHS Improvement and the inclusion of their role as a 'safety action' in NHS Resolution's maternity incentive scheme.
When things do go wrong, participants in our NHS co-production meeting reiterated the importance of trusts being transparent and involving families in any investigations. This was a key recommendation of Each Baby Counts, and NHS Resolution’s guidance Saying Sorry. It also echoes the findings of a number of CQC reviews, including ‘Learning from serious incidents in NHS acute hospitals, Learning, candour and accountability’, and ‘Opening the door to change’, all of which highlighted the importance of being open and honest when things go wrong.
In services rated as outstanding, we found a culture in which reporting was valued and encouraged, with feedback to those who made reports and shared learning from the investigations. They also provided staff with training on recognising and reporting patient safety incidents. In addition, in these trusts there were clear lines of communication between frontline staff and senior leaders, with audit and risk management processes that were well embedded. Since 2017 the Healthcare Safety Investigations Branch (HSIB) has been carrying out investigations into maternity incidents and this work will be a valuable source of learning.
The 2019 NHS Patient Safety Strategy focuses on the importance of staff recognising and reporting safety incidents in order for learning from incidents to be effective. What determines whether this truly occurs in individual services is the quality of the leadership and the culture it engenders. We continue to monitor learning from incidents as part of our inspections. More broadly, we have found that trusts who encourage a culture of learning and openness alongside a willingness to listen to and prioritise the needs of the women using their services are more likely to deliver care that is not only safe, but person-centred and empowering.
Individual staff competencies, teamworking and multi-professional training
When urgent action is required to respond to an emergency, it is critical that teams can work together well, and have the knowledge and skills to manage fast moving situations effectively. This can only happen if the whole team is prepared and regularly trained to recognise and manage different types of emergency.
It is positive that prioritising and investing in the capability and skills of the maternity workforce, and promoting effective multi-professional team working, are key elements of the national ambition to improve maternity care. However, maternity training still varies widely – both in terms of topic areas covered and resources available.
There are three elements that we believe need to be addressed in terms of training:
- core competencies of individual members of staff
- effective teamworking between different staff groups
- scenario training that role plays planning for serious complications that require an effective multidisciplinary team response
The combination of these elements should help to make sure that women receive high-quality support that will recognise and respond to any changes in risk during their antenatal, intrapartum and postnatal care.
The inspection reports we reviewed included examples of trusts who had considered and addressed training needs – but also examples where staff did not have the skills and competencies that their roles required, and where teams did not work effectively. Every maternity service must ensure that the range of training matches the identified needs for their service.
There is especially strong evidence to highlight the importance of regularly updated training in fetal heart monitoring – delivered in a multidisciplinary setting that covers team working and situational awareness as well as use of equipment.
The Royal College of Obstetricians and Gynaecologists’ (RCOG) Each Baby Counts report found that in 74% of babies where improvement in care might have improved the outcome, fetal monitoring was identified as a critical contributory factor. NHS Resolution’s Early Notification scheme progress report also showed similar findings. And NHS Litigation Authority’s analysis of 10 years’ of maternity claims found that cardiotocograph (CTG) monitoring was the sixth most frequent category of claim and the second most costly to the NHS in terms of value of claims paid out. The increasing cost of maternity claims is a continuing concern, but what cannot be quantified is the human cost behind these figures and the lasting trauma to mothers, babies, families and staff.
We have particular concerns about the frequency and quality of multi-professional scenario training. We have seen evidence that some obstetric staff working in maternity units that have low numbers of deliveries are not able to maintain the relevant clinical skills and competencies. This is an area that requires urgent attention at trust and national level. Positively, we have seen some innovative examples of trusts addressing this through rotational joint appointments that are shared between large and small maternity units.
But it is not just about cross-professional training for maternity staff. During our NHS co-production meeting, representatives from a number of NHS ambulance services flagged how valuable it was for them to also be involved in multi-professional scenario training. In particular, they mentioned the importance of this in terms of transporting women in labour from the community. The establishment of Local Maternity Systems should provide opportunities to share access to training from the wider cross-professional workforce and for those working in smaller teams.
As part of our regulation of services, we will continue to review the impact of workforce issues, including the effectiveness of training and staffing pressures, on the safety and quality of maternity services.
Active engagement with women using maternity services
Seeking ways to listen to and learn from the experiences of women who have used maternity services is vital to improving and developing services.
CQC carries out a regular survey of women who have used maternity services to gather information on their experiences. The 2019 maternity services survey highlighted that while most women felt that they received high-quality maternity care, there were areas for improvement. These included perinatal mental health and access to help and support outside of acute settings.
Only just over half of women surveyed reported that midwives appeared to be always aware of their medical history during their antenatal check-ups. This is an area that services should explore as it is crucial to assessing risk and planning appropriate management throughout pregnancy.
As has been the case in previous years, scores for questions about postnatal care remained particularly poor with information provision, emotional support and communication after birth all highlighted as areas where experiences could be improved.
Each of the 126 trusts in England that took part in the survey received the individual results for their trust, and we expect trusts to use the results of the survey to inform discussions on how to improve local maternity services.
Services need to ensure that they proactively engage with their local population to define their priorities, and make sure that women are at the centre of their vision and service. To support this, NHS England and NHS Improvement champions Maternity Voices Partnerships. These partnerships bring together women and their families, commissioners, and midwives and doctors to review and contribute to the development of local maternity care. Working with Maternity Voices Partnerships to coproduce local maternity services is a ‘safety action’ in NHS Resolution’s maternity incentive scheme.
Conclusion
The work underway to improve the safety of maternity services is welcome, but our inspections have found there is more that needs to be done to ensure that women and babies get consistently safe care.
This briefing highlights three key areas for improvement:
- the development of the board level maternity safety champion role is crucial to ensure a proactive approach to the maternity services that the organisation provides
- the issues of staff competencies, teamworking and training will require support from professional organisations and regulators. We welcome the launch of NHS England and NHS Improvement’s Maternity Safety Support Offer self-assessment tool, which will allow maternity services to benchmark themselves against good and outstanding services
- finally, we want to see evidence from all providers of maternity care that there is true engagement and involvement with individuals and groups who use maternity services through Maternity Voices Partnerships
We will be further developing our key lines of enquiry for maternity services so that we are able to better assess how trusts plan, provide and assure the delivery of high-quality, patient-focused maternity care. And we will continue to review the impact of workforce issues, including the effectiveness of training and staffing pressures, on the safety and quality of maternity services, and to call these out when we see that these issues are impacting on the quality of care for woman and babies.
As a member of the National Maternity Transformation Programme, CQC will continue to support the implementation of the Maternity Safety Strategy which includes development of networked maternal medicine services and taking forward the recommendations from the Neonatal Critical Care Review.
In addition, we will be strengthening our relationships with key partners including RCOG and the Royal College of Midwives (RCM). We will be seeking not only to share information more effectively, but to better understand factors that might act as barriers to the provision of good care, with RCOG’s research into improving team dynamics in obstetrics and gynaecology of particular interest (Mountfield J, ‘What must be done about bullying and undermining in obstetrics and gynaecology’. Obstetrics, Gynaecology and Reproductive Medicine, Volume 29, Issue 7, 207–208).
Safe maternity care is not an ambitious or unrealistic goal. It should be the minimum expectation for women and babies – who should also be receiving care that is person-centred, supportive and empowering. Improvements in safety still need to be made to ensure that this is the case for everyone, every time. Five years after the Kirkup report, we have not found that the changes needed or the change in safety culture we have called for have been consistently delivered. Leadership and cultural barriers need to be addressed if these overdue improvements in safety are to be achieved with the urgency needed.
Contents
Figure 1: Maternity safe ratings from first rating to current
Governance, leadership and risk management
Individual staff competencies, teamworking and multi-professional training
Active engagement with women using maternity services
See also
News story: CQC briefing on improving safety in NHS maternity services