North Tyneside Council: local authority assessment
Overall summary
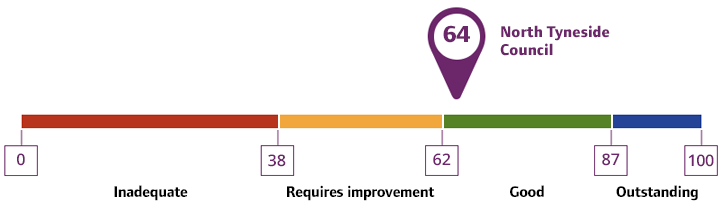
Local authority rating and score
Quality statement scores
Summary of people’s experiences
Feedback from people in North Tyneside on their experience of accessing adult social care services was mixed. Many people and unpaid carers felt more clarity was needed to support people’s understanding of the strategic work the local authority was undertaking and how they led to the delivery of meaningful outcomes for people and unpaid carers. The local authority had coproduced several improvements at the time of our assessment, but this needed time to embed before allowing analysis of the impact of these changes.
People told us Care Act assessments were conducted professionally, using strength-based approaches, and focused on whole-family support to ensure people could live at home for longer. However, they also told us they waited a long time for assessments of longer-term support needs, and there were considerable delays in annual reviews. Longer-term needs were assessed after the initial 6 weeks support offered by the council post-hospital discharge. Unpaid carers said the local authority were good at providing crisis and urgent care, but there were delays in assessments and reviews, long waits for services to start, and confusion about assessment processes for transitions between short-term and long-term support.
National data and feedback from unpaid carers were mixed, with a lack of contingency planning and access to respite services a particular point of comment. National data provided by the Survey of Adult Carers in England (SACE 2024) showed 25.00% of unpaid carers in North Tyneside were accessing support groups or someone to talk to in confidence. This was tending towards a negative variation to the England average of 32.98%. The local authority had recently invited the voluntary and community sector to carry out an extensive survey of the services available to unpaid carers in North Tyneside, leading to several changes to processes and increased respite provision in the area.
The local authority had clear priorities and a focus on prevention and early intervention, with a number of integrated services available to support eligible and non-eligible needs. However, people told us they were often unclear what the local authority support offer was, or how to access it. People felt there could be more information and services available relating to health and fitness.
People’s feedback around hospital discharges and the intermediate care, rehabilitation, and enablement offer in North Tyneside was positive. The local authority’s ‘home first’ approach had seen a shift away from residential services to looking at assistive technology and equipment to support people to continue to live more independently at home or in community-based services such as extra care. Data provided by the local authority, collated to help support understanding of people’s outcomes following support from reablement services, demonstrated improvements in mobility and selfcare indicating reablement intervention had been beneficial and contributed positively to most people’s quality of life.
People told us waiting times for occupational therapy assessments had increased in the past 12 months. The local authority had responded through a restructure of the service, including the use of Trusted Assessors and quick turn-around processes for common equipment requests. However, at the time of our assessment these changes still needed time to embed.
Direct payments were recognised across the board as an area of development for the local authority, with people telling us of low uptake, delays in implementation, confusing processes, and a shortage of Personal Assistants (PAs). The local authority had introduced initiatives to address this, including raising awareness in the community through coproduction groups and a drive to improve the personal assistant offer in the area.
There was a strong focus on health and prevention needs for the people in North Tyneside. The impacts of deprivation on mental health and for those people with multiple complex needs such as homelessness and drug/alcohol abuse were well known, and joint initiatives were in place to support communities who traditionally struggled to access adult social care support.
An ageing population with ongoing and complex health needs, and an increasing number of younger people with mental health, learning disabilities and autism had led to the local authority reviewing their supported accommodation offer within North Tyneside. People told us access to services was typically good, though there were some issues with the quality of homecare services.
People told us the local authority had strong partnerships with health, the voluntary and community sector, and housing, supporting key preventative and early intervention services. Access to the local authority was made easy through digital and face-to-face options based in the community and at local hospitals. The commissioned review of support for unpaid carers identified areas of development, including greater focus on social isolation and transitions for young carers. People told us communication between the local authority and health partners around Continuing Health Care (CHC) funding could be improved.
People told us there was a lack of consistency in the process for transitions from children to adult services. This was also true for people with mental health needs transitioning into community settings following time spent in hospital. The local authority had reviewed their transitions processes and introduced a co-productive Transitions Advisory Group (TAG), as well as the new role of Transitions Lead to improve consistency across all transitions.
Data provided by the local authority analysis of their Making Safeguarding Personal targets showed only 67.15% of people who raised a safeguarding concern were asked about the outcomes they wanted from the subsequent enquiry. However, 95.70% of those people asked, felt their outcomes had fully or partially been achieved. Deprivation of Liberty Safeguards (DoLS) assessments had been an issue in recent years, with prolonged delays in process and a lack of trained staff to complete the necessary paperwork. Recent additional support, including the use of independent Best Interest Advisors (BIAs), and administrative changes to the paperwork process had led to a reduction in waiting times.
People told us there were strong coproduction processes in place, particularly in the last few years, with examples of people with lived experience of care and support services involved in strategic and operational decision making. People told us senior leaders were friendly and approachable, but worried about succession planning and loss of key staff, telling us of ‘corporate memory’ and how information, and strong partner relationships could potentially be ‘lost’ when long-term staff moved on.
Summary of strengths, areas for development and next steps
North Tyneside had a long history of supporting local communities. The decline in shipbuilding along the riverside, and coal mining in the north and west of the borough, left a legacy of significant poverty. Our assessment of the adult social care function in North Tyneside took place during a time of ongoing transformation. The restructure of the adult social care directorate had begun in 2023 and was taking longer than originally planned. This was to ensure governance processes led to clear outcomes for people accessing adult social care services.
Staff and leaders told us meeting the needs of a rapidly ageing population was a key focus for the local authority, leading to increased investment in prevention and early intervention services, as well as a ‘home first’ approach to reablement and rehabilitation support. Community-based support also focused on the increasing number of young people with complex needs transitioning from children’s services into adulthood.
Data provided by the local authority showed waiting times for assessments and reviews had been lengthy in 2023-2024. Partners and providers felt frontline teams were slow to respond to changing needs. Extensive work by the local authority, including staff recruitment and training as well as robust processes for prioritising assessments and monitoring workloads had led to a significant reduction in waiting times for both assessments and reviews by the end of 2024.
According to a voluntary and community sector survey commissioned by the local authority in 2024, feedback from unpaid carers indicated the health of those they cared for was declining, resulting in greater care needs and increased demands on unpaid carers. The local authority responded by working with unpaid carers and partners to improve the support available to them, including access to information and advice, access to respite support, and links to the Care and Connect service which was a community-based service promoting people’s health and wellbeing.
Feedback from staff, leaders, and partner organisations highlighted direct payments as an area of focus for the local authority. Staff told us they were often reluctant to offer direct payments because processes to set up direct payments were cumbersome and difficult, and the complexity made it easy to make mistakes. Senior leaders told us they had streamlined the direct payment process and refreshed staff training to improve confidence and competence in completing direct payments assessments. This, combined with focused work supporting unpaid carers to access direct payments was felt to be improving outcomes for people, including through one-off payments for essential equipment and services.
Partners told us local authority frontline teams and support services enabled effective hospital discharges, with rehabilitation and enablement services identified as particularly good at promoting people’s independence and reducing the need for hospital readmissions. Staff and leaders told us a recent review of ‘step-down’ services led to a move away from residential support to more community-based extra care modelling.
Recent changes to the way occupational therapy and the provision of equipment were managed within the local authority and their partners had led to improved outcomes supporting the home first and preventative approaches key to the new ways of working in North Tyneside. Whilst it was too soon to assess the full impact of the changes, the initial feedback from staff and providers was positive.
The recent Joint Strategic Needs Assessment (JSNA) and Market Position Statement set out the current and future health and adult social care needs of local communities, with a move to home and community-based support enabled by a series of supported accommodation and homecare review and retendering processes. Partners told us a regional approach to future supported accommodation was being explored and a review of current homecare provision locally aimed to improve the offer for hard-to-reach areas.
Partners and staff told us there were strong relationships with stakeholders. Those relationships had been built up over an extended period and allowed for constructive challenge when difficult conversations were needed. There were clear strategic links and processes for sharing information both at a local and regional level, including working towards the new North-East combined authority. There were strong integrated service relationships with health partners using pooled resources to meet joint strategic priorities.
Gateway, Care Point and Care and Connect services were used as front-door first contact and triage support, linking with health, voluntary and community services as well as crisis support teams to ensure immediate needs and low-level support services were accessed quickly and effectively.
Feedback on transitions was mixed, but the local authority had reviewed and implemented a number of changes to improve outcomes, including a new Transitions Advisory Group and the recruitment of more Approved Mental Health Professionals (AMHPs) to support mental health hospital discharges.
Staff told us there were safeguarding enquiries open longer than expected, leading to a potential for ongoing risks and concerns for people’s safety. There were good partnership working arrangements and learning from Safeguarding Adult Reviews (SARs) at local and regional levels. Senior leaders told us there was a clear understanding of local safeguarding risks and issues, with a focus on self-harm, alcohol and drug misuse, and homelessness.
People, staff, and partners felt the local authority learned from feedback about their experiences of care and support. There were processes to ensure learning happened when things went wrong, and from examples of good practice at a local, regional, and national level. Leaders encouraged reflection and collective problem-solving, and staff told us they felt valued and included in decision making.