North Somerset Council: local authority assessment
Overall summary
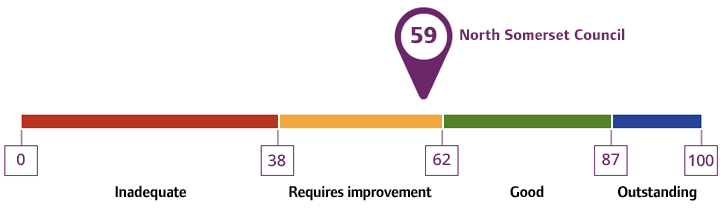
Local authority rating and score
Quality statement scores
Summary of people’s experiences
People in North Somerset had mixed experiences with the local authority care and support services, reflecting both positive and negative outcomes.
Feedback from unpaid carers was mixed. Some carers reported positive experiences with staff and services, for example, one carer told us they were listened to and was offered choice in support with their caring role. In contrast, other carers had negative experiences in relation to availability and outcome of assessments, access to respite and accessing timely and appropriate support. Lengthy wait times for assessments and reviews impacted on carers’ wellbeing and ability to provide care. Several carers expressed their needs were not adequately recognised or addressed, resulting in feelings of being unsupported and overwhelmed. Some carers from minority ethnic communities reported additional barriers due to language and cultural differences.
People’s experiences of assessments, care planning and reviews were mixed. Some people told us they received strengths based and person-centred assessments, highlighting the helpfulness of staff. However, some found phone-based assessments impersonal and felt they lacked sufficient focus on individual needs. While concerns were promptly resolved in some cases, others faced dissatisfaction with assessment practices. Some described assessment processes as impersonal, and others felt their or their loved ones’ needs were not assessed holistically, with long-term goals and independence support being overlooked. Feedback from carers ranged from positive experiences to concerns about limited choices and access arrangements for communication and support.
Some people were not always aware of preventative measures, feedback was mixed on the knowledge of community resources and information shared. Wait times for assessments and reviews were not always timely. People’s and carers’ needs reported positive impacts of preventative approaches, others described challenges related to wait times and effectiveness of support with alternative solutions. In relation to technology enabled care (TEC), while some people reported positive experiences of technology enhancing their care, others highlighted challenges of access and effectiveness, particularly for older adults.
People’s experience of access to information and advice was mixed. While some people found information easy to locate, others described it as challenging to access and navigate the local authority website. Some people reported having difficulties contacting the local authority and accessing clear information relevant to their care. People reported that their experiences improved once contact was made with the local authority’s Single Point of Access (SPA) service and relevant teams.
People reported mixed experiences of multi-agency support. While integrated teams facilitated service access and promoted independence for some, access to certain services, such as day services and respite, remained limited, particularly in rural areas. Transition experiences between services, including children’s to adult's services, were mixed, with some positive outcomes and challenges reported. While most people felt safe, the consistency of contact following safeguarding referrals could be improved.
Summary of strengths, areas for development and next steps
In 2023, following a restructure, the local authority integrated adult care services and housing into a single directorate, including those previously under Public Health.
Carers support was a key area for development. The needs of unpaid carers were central to market shaping, seen in the development of the All-Age Carers strategy 2024/2028 and there was a focus on trying to improve the offer to carers.
Waiting lists delayed people accessing support. The local authority used various strategies to manage wait times, including internal audits, targeted initiatives such as ‘Team Effort Days’ and a ‘waiting well project’, and proactive monitoring of waiting lists. Risk-based allocation of tasks prioritised urgent referrals, with clear communication channels to direct people to alternative support where appropriate. New technologies and projects aimed to streamline processes and reduce delays. While improvements were seen in several areas, some delays remained. Joint working with children's services ensured timely support for transitions.
People could not always access the support information they needed. The local authority had acknowledged these challenges and had worked to develop a varied range of information in accessible formats. A senior leader told us about improvements like the Better Health North Somerset website had enhanced accessibility to resources and promoted user-friendly trackable referrals.
The Technology Enabled Care (TEC) and Reablement Intervention (TRI) team adopted the model of strengths-based practice to support person-centred assessments and deliver outcome focused support for people. For example, staff told us they were ‘proud of their approach to assessment and care planning’. They described an approach which ‘reflected what the person values and what’s important to them’ to demonstrate the team’s understanding and practice of strength-based working. Frontline teams were proud of the outcomes they achieved with people to promote independence.
The local authority had recognised through staff feedback and ‘learning together’ audits, an over-reliance to offer commissioned support to people with new or short-term care and support needs. In response they had introduced a new ‘Eligibility Resource Forum’ (ERF) to support staff to be more creative with how they might meet peoples short term needs with ‘time to think’, this was mandatory before a commissioned home care or care home package was agreed by managers. Staff and senior leaders told us the ERF considered a range of ways to meet eligible and non-eligible needs, ‘not just the quick resolution’, by suggesting preventative services as an alternative to commissioned care, this would further promote a person’s own strengths, resilience and independence. Multi-disciplinary teams would attend the forums twice weekly when cases needed review, as a quality assurance mechanism to ensure eligibility for assessments and consistent application in the process for adult social care eligibility and resource allocation.
The local authority worked with people and partners to improve people's experiences and outcomes. For example, they actively promoted co-production, embedding this approach throughout their work to ensure that services were shaped by those who use them. Despite these efforts, we heard mixed feedback from carers, however, there was some positive feedback shared of the co-production groups. People involved told us that they saw value in the way the local authority listened carefully to the views of people who draw on services and their carers separately, as this had given carers the opportunity to have their say. The local authority had taken steps to increase carers on the Carers Partnership Board and involved them in co-producing the carers strategy. The strategy was completed in 2024, and carers continued to play an active role in delivering the action plan. To support sustained representation of lived experience within the Carers Partnership Board. Those involved told us they felt the local authority was committed to hearing their views and contributions and they were excited about co-production opportunities. The local authority shared ideas and best practices to improve care across the region, which showed their commitment to growth, inclusivity, and excellence in adult social care.
There was a need to better integrate adult social care priorities with preventative services. The local authority had introduced a new prevention offer focusing on targeted interventions for people at risk. This initiative aimed to improve people’s wellbeing by considering the impact of professional actions, performance, and decisions. However, improvements were needed to ensure all people at risk of future care and support needs could access the services and information available. Existing early intervention and prevention (EIAP) services included a handyperson service, reablement, falls and frailty pathways, carer support, dementia day services, TEC, and first response services. The long-standing in-house meals service supported those with minimal care needs experiencing difficulties preparing food. These were valued by staff as having a positive impact on well-being outcomes for people.
The local authority demonstrated a commitment to several positive initiatives, including a multi-agency approach to initial contact and service navigation, various preventative services which included the occupational therapy offer and jointly commissioned OT equipment service, offering residents the opportunity to see and try equipment and TEC products. There was a strong emphasis on TEC development. The local authority showed a commitment to staff training and development and had a visible leadership team dedicated to service improvements.