East Riding of Yorkshire Council: local authority assessment
Downloads
Overall summary
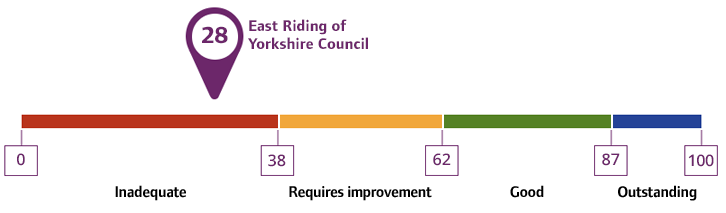
Local authority rating and score
Quality statement scores
Summary of people’s experiences
We found many people experienced delays in accessing services which affected their experiences and outcomes. There were delays for assessments, reviews, and equipment assessments, including sensory support. While people waited, their needs sometimes escalated, meaning some experienced crisis which risked their wellbeing. However, when people received services in the East Riding, they generally experienced strength-based, person-centered practice that accounted for their needs. National data indicated most people who received support had control over their daily lives and were satisfied with care and support. However, this was not the experience of the majority of people due to difficulties accessing care.
There were delays in timely safeguarding enquiries. While people at highest risk were generally supported quickly, local authority information indicated people experienced delays in enquiries, some disjointed processes, and a lack of confidence and capacity in local authority staff.
Carers in the area who were known to the local authority’s dedicated team received services that accounted for their needs, understood the challenges they faced and supported them to care for their loved ones. There was ongoing work to improve the reach of the offer and communication around the support available to help more carers in the area access support.
There was limited reablement care available to support people following discharge from hospital. Fewer people were likely to return to independence or achieve reablement goals because of this. While there were some services available in the community that could support people to remain independent at home, our assessment found the local authority did not support people sufficiently to promote healthier lives and independence.
Some people told us their preferred inclusion and accessibility arrangements were not always followed. There was not enough focus or understanding of the experiences of people with protected characteristics within the local authority to ensure people could equitably access services and achieve the outcomes that were important to them.
There had been significant issues with the capacity of service providers to meet the needs of people in the East Riding. This persisted for some people. Some people in rural areas were more likely to experience significant delays to their care. In some cases, issues were so severe people who could have returned home following a hospital stay had been unable to due to a lack of capacity. More people stayed in residential care provision than needed for longer.
Some people told us they had to complain to get their voice heard. There were some key issues in the information provided to people and the process around paying for care that the local authority was resolving at the time of our assessment. More people were involved with the local authority’s efforts to hear people’s experiences to design and deliver services. There were a number of partnership boards in place that supported people’s voice.
Summary of strengths, areas for development and next steps
People’s care and support had not always reflected their right to choice and reviews could be difficult to instigate. Communication could be limited. The local authority did not have a practice framework in place at the time of our assessment to support a unified and cohesive adult social care system in the local authority. Staff demonstrated strengths-based and person-centered practice when completing assessments, developing care plans and reviewing people’s needs though difficulties in accessing care meant this was not the majority of people’s experience. There was mixed feedback about the availability of training that allowed staff to develop their skills and knowledge. Some quality assurance of activity took place though this was primarily focused on case file audit and not linked to a wide range of quality assurance activity. This limited opportunities to ensure quality within wider service performance, risk and external benchmarking.
People waited for assessments or services, though this was based on risk. People at higher risk were generally responded to quickly. Where needs were identified at the point of initial contact, staff could engage some services in the community to support people while they waited. Where people waited, processes had been recently updated to ensure regular reviews to identify if need or risk had changed. However, this wasn’t always effective, and staff described supporting people in crisis. Where these processes had been updated, it was too early to evidence sustained impact.
Staff, partners, people and leaders identified there was more to do to hear from and support seldom-heard communities. There were several examples of the way staff worked with people to meet their needs in respect of their culture, background, and experience. There were, however, some instances where non-verbal communication wasn’t always well supported and there was a lack of services available for people from Eastern Europe and Ukraine, despite increasing populations. The intersectionality of people’s protected characteristics was not always well understood. Staff had been open about wanting to be more confident to support people from different protected characteristics groups. The local authority had developed a bespoke workshop that was being expanded at the time of our assessment. There was positive commitment to support the prison population through a dedicated team that was improving their experiences and supporting effective release planning. The local authority had limited data about the protected characteristics of their adult social care population which affected their ability to understand people’s experiences and outcomes. There was a lack of local strategy and action to reduce inequalities in people’s access to care and support, their experiences and outcomes.
Intentions for the care market in East Riding were often unclear. There were limited clear plans in place about the requirements for the market, including the types and amount of services needed. This created an unclear picture for providers in the area about the local authority’s commissioning intentions. Quality monitoring of providers had been limited to reactive reviews and there was recently identified work ongoing to visit the 24 care providers who had not been seen in the last 5 years. Capacity within the care market was a significant concern. People faced a lack of home care provision, resulting in short-term residential care that was often extended. We heard several examples of when short-term residential care became permanent as a result of capacity issues within the market. While the majority of people were placed out of area due to choice, the local authority identified there was a disproportionate number of working age and younger adults placed out of county due to a lack of provision. There were also gaps in complex nursing and dementia care.
The partnership with the mental health NHS Trust in the area was working well and investment in senior social workers within the structure had continued to strengthen the relationships between services to support Care Act duties. Operational partnerships with hospitals could be challenging due to the arrangements of health services outside the area. However, there were some concerns that disagreements or delays in partnership funding delayed people’s care and support. This meant some people were not discharged from hospital or did not receive the care and support they needed to best support their independence and long-term outcomes in a timely way.
There were positive arrangements to support young people to transition from children’s to adult’s services which had improved people’s experiences. There were examples of working with partners to develop community safe spaces, such as the Wellington Road Community Hub in Bridlington, to meet partnership objectives and deliver services for people who needed them most.
The local authority’s safeguarding model changed to a ‘hub and spoke’ approach about a year before our assessment. There were increased numbers of safeguarding contacts in recent years. The number of safeguarding enquiries (section 42 enquiries) had remained consistent. Some partners felt there was more guidance needed to help them make appropriate contacts and that this training and guidance had dropped off since the change in approach.
The local authority was generally supporting people at highest risk in a timely way. Most people who received care and support said they felt safe. However, there were delays to timely enquiries for people at lower risk. This was primarily as a result of a lack of capacity within local authority teams. There was a lack of confidence to deliver section 42 enquiries from some teams. Use of advocacy was low to support people who lacked capacity. The local authority had committed to a review of their safeguarding model as a response to staff and partner concerns about the approach.
There was a waiting list for Deprivation of Liberty Safeguards applications in the area as a result of a corporate vacancy management process. A lack of staff had created a risk that people’s safety and human rights were infringed.
Information security risks existed within local authority data systems which included a reliance on a variety of spreadsheets to manage work a case management system should be able to handle. Staff spent time duplicating across systems, and there were risks information was lost or misplaced in these instances. Work was progressing to improve recording systems.
Several significant leadership changes had taken place over recent years which affected the local authority’s priorities, strategies and plans. There were also impacts on some partnership work and staff said leadership had not been visible. Key mechanisms, such as overview and scrutiny committee, corporate risk management and data intelligence, were not considered closely against the local authority’s Care Act duties. Some key strategies were delayed or non-existent. These factors limited the local authority’s governance and strategic planning to create the environment to deliver the best possible outcomes and experiences for people in the East Riding.
There were many areas of challenge identified in this report that were understood by the senior leadership team. The local authority had identified the need to draw on external support to improve across several areas though much of this was at too early a stage at the time of our assessment to evidence progress and impact.