Contents
Defining an ethnic minority-led GP practice
- Do ethnic minority-led practices have poorer ratings?
- Are ethnic minority-led practices more likely to be inspected?
- Do ethnic minority-led practices have a differential experience of the inspection process and outcomes?
- Factors internal to ethnic minority-led practices
- Factors external to ethnic minority-led practices
- Internal CQC factors
- Action to ensure equity of treatment for practices and to benefit patients
- Factors outside of CQC’s role where we could use our influence
Conclusion: Learning from what we found
- Appendix A: Statistical model for ratings
- Appendix B: Terms of reference for the sub-group of the Primary Care Quality Board
- Contributors
Summary
The Care Quality Commission (CQC) is committed to being a fair regulator. We consider equality for the organisations that we regulate, for people using health and adult social care services, and for our own workforce. We embed assessments of organisational and health inequalities across all aspects of our regulatory activity.
Providers led by GPs of an ethnic minority background have raised with us concerns that they do not receive the same regulatory outcomes from CQC as providers led by GPs of a non-ethnic minority background.
To investigate and respond to these concerns, we started a programme of work in February 2021. The focus of this has been on how our own regulatory approach affects ethnic minority-led GP practices and how we can improve our methods to address any inequalities we identify.
Our review used both quantitative and qualitative methods. These comprised reviews of our data and processes, an online community of 36 ethnic minority GPs, a survey of 771 GP practices, a survey of 57 CQC inspectors and focus groups with CQC inspection teams (attended by eight inspectors, four inspection managers and four GP specialist advisors). We engaged with key stakeholders, including subject matter experts, on our processes and findings.
The aim of our review was to understand the experiences of ethnic minority-led GP practices, rather than to reflect the experiences of all GP practices. It is important to note that because of the methods we used in this research, the results are reflective of the people who participated in our online community or responded to our surveys. Only ethnic minority GPs were invited to take part in the online community and so the views expressed in that forum may apply equally to non-ethnic minority-led GP practices. The aim of the online research community was to understand lived experiences of ethnic minority GPs, rather than to reflect and compare GPs’ experiences.
Regulatory outcomes and experiences of ethnic minority-led GP practices and the factors associated with them
Due to limitations in the data available to us from all partners in the system, we were unable to fully explore the nature of the relationship, or existence of any causal link, between ethnic minority-led GP practices and regulatory outcomes such as ratings and frequency of inspection.
Ethnic minority GPs in our research reported poor experiences of the inspection process and its outcomes. In our online research community of ethnic minority GPs, there was a feeling that their inspection outcomes could be “harsh” and “unfair”. They felt that CQC does not understand or appreciate the unique challenges that ethnic minority-led practices face.
In our survey of GP practices, ethnic minority-led practices were more likely to report that GPs in their practice experienced adverse impacts on their physical and mental health, a negative impact on their personal and/or family life, and had seen an increase in staff sickness as a result of the inspection process.
However, in this survey, ethnic minority-led practices were more likely to report that the quality of care improved following a CQC inspection.
External system factors
Most ethnic minority-led practices in our GP practice survey served populations with a high proportion of socio-economic deprivation. Both GPs and CQC colleagues identified socio-economic deprivation as a challenging factor, as it can affect the practices’ ability to achieve national targets that we use in assessments of quality, such as the uptake of immunisations or screening among patients. Some inspectors and specialist advisors felt our approach did not recognise enough the surrounding context of practices, and that some practices are disadvantaged for not achieving similar outcomes to those with very different contexts and patient communities.
The online community of ethnic minority GPs identified that deprivation also presents other challenges, such as increased workloads, as patients with poorer health typically need more care. These practices also experience difficulties with recruitment and funding. This makes it harder for practice staff to cope with patient demand, which again can have a potential impact on CQC regulatory outcomes.
Our online community also highlighted a perception of a lack of leadership support for ethnic minority-led practices from external bodies. In addition, some ethnic minority GPs reported experiencing racism from patients, especially when patient expectations could not be met. They also felt patients were more likely to raise a complaint about an ethnic minority GP than a White British GP.
Internal practice factors
Our survey of GP practices showed that certain types of practices are more commonly associated with being ethnic minority-led – for example, single-handed or individually led practices. We heard from our online community and in focus groups and interviews with inspection colleagues that it can be harder for smaller practices to spare the time needed for an inspection. In the focus groups and in the online community, we also heard that these practices experience professional isolation.
Responses from CQC colleagues also highlighted factors relating to practice management or leadership, including less familiarity with CQC regulation or poorer IT skills, reducing the ability to provide evidence at inspections. This may reflect a need for CQC to be more considerate of these differences to better support practices.
CQC factors
GPs in our online community felt that CQC’s need for objectivity potentially had a negative impact on ethnic minority-led practices and could lead to unfair outcomes, because methods are not able to be tailored to reflect providers’ circumstances.
There is a perception that the evidence used in inspections is a disadvantage to both ethnic minority-led practices and practices serving socio-economically deprived patient populations as the differing views of patients, such as a reluctance to receive vaccinations, affected practices’ performance when compared against national targets. Similarly, inspection colleagues and specialist advisors felt that website reviews and online feedback forms could disadvantage practices serving communities with lower levels of English proficiency.
CQC colleagues emphasised that their key priority was to ensure that care was safe and accessible, regardless of the challenging circumstances that practices might face. However, both CQC inspection teams and GPs raised concerns that CQC did not always take into account the innovations that practices had developed to respond to local needs.
Inspection colleagues and GPs thought that CQC’s terminology can impede ethnic minority-led GP practices from meeting data requests and regulatory requirements. Ethnic minority GPs in our online community highlighted a need for clear, transparent and accessible guidance as the lack of clarity may affect inspection outcomes.
Processes to challenge regulatory outcomes and ratings were also noted to have an impact on ethnic minority-led GPs, with some ethnic minority GPs in the online community perceiving a possible risk of victimisation, poorer ratings or re-inspection if they choose to raise complaints.
Ethnic minority GPs in the online community also raised the composition and skillset of inspection teams as an issue, feeling that inspection teams needed greater cultural competence, and an understanding of local areas and populations.
Improvements that could help promote equity in regulatory outcomes
Improvements for CQC
Both GPs and inspectors who responded to our surveys felt there could be more in CQC’s methods to reflect the specific context within which GP practices operate. They said that inspection teams should gather a wider range of evidence about how a GP practice meets the needs of its populations, including how the practice is reducing health inequalities. In the focus groups and interviews with CQC colleagues, we heard that this would help to recognise more responsive care and good leadership where a GP practice is operating in more challenging circumstances. It was also felt that inspection reports could reflect that lower ratings may be because of additional external pressures, rather than poor clinical work or a lack of concern by the practice for the wellbeing of its patients.
Ethnic minority GPs in our online community wanted to see a more supportive approach from CQC, better communication from inspectors and greater transparency about expectations, processes and decision-making.
By encouraging practices to engage more with our guidance and support, we can help them understand regulatory requirements and expectations. Practices felt a more collaborative approach would support providers and patients alike, as providers could discuss concerns without fear of repercussions, helping them work with CQC to improve.
Improvements for the wider system
A consistent theme from ethnic minority GPs was about the need for more support from the wider system. There was agreement that support from clinical commissioning groups (CCGs) can help a provider to improve, but in the GP provider survey, ethnic minority-led GP practices reported lower levels of good support from CCGs. In the online community, other partners in the system, such as the British Medical Association, General Medical Council and NHS England and Improvement, were also highlighted as having a role.
Inspection teams generally considered that the role of supporting providers sat with CCGs as opposed to CQC. However, some inspectors had experience of where CCGs had not acted to support GP practices as the CCGs thought it was CQC’s role. This suggests a lack of clarity about roles and responsibilities around supporting GP providers. It was suggested that CQC and CCGs needed to improve their working relationship and increase dialogue about the support practices need. It was felt that improving this relationship should not be the responsibility of individual inspectors.
What we will do
This programme of work was designed to look at our own systems and processes and how these affect inspection outcomes for ethnic minority-led GP practices. The findings show that there is work for us to do to ensure we achieve our strategic and equality objectives and deliver our core purpose to ensure we encourage practices that need support to improve.
The work has identified an inter-relationship between factors that can lead to poorer regulatory outcomes. Internal or practice factors often have a disproportionate impact on practices where many ethnic minority GPs operate. Ethnic minority-led GP practices are often operating single-handedly, which results in challenges in support, resourcing and capacity. These additional burdens affect the ability of a practice to show evidence that it is meeting regulatory requirements.
Importantly, there are also wider, contextual factors that affect ethnic minority-led GP practices – in particular the efforts required to respond to the health inequalities of patients in areas of deprivation. Practices in areas of deprivation struggle with lower funding and systems of support. This work has demonstrated the need for better system-wide engagement in addressing these factors and we hope to further this conversation through the findings from this report.
We will take the following actions to respond to the findings from this review:
- Continue our work through the Regulators' Pioneer Fund to support us to identify innovation in areas of deprivation and share good practice as part of our routine regulatory processes, assessments and engagement.
- Develop our approach to our new duty to review and assess integrated care systems, including a need to reduce inequalities for people who use services. In doing this, we want to address where local systems need to provide more support to ensure that primary care meets the needs of everyone in their population.
- Continue to work with our system partners in the sub-group of the Primary Care Quality Board to identify and progress shared priorities in ensuring equality for ethnic minority-led GP practices and the populations they serve. This includes:
- Reviewing what can be done within the wider system to ensure that single-handed practices are not unduly disadvantaged by the circumstances in which they work.
- Reviewing whether the current arrangements for supporting GP practices are effective for those in areas of deprivation that are experiencing disproportionate pressures, such as professional isolation and lack of funding.
- Reviewing and improving ways to capture feedback from diverse ethnic groups about the care they receive.
- While continuing to expect good quality of care for everyone and without compromising on expected standards of care, we will strengthen how we consider the context in which a GP practice works. This can include:
- Gathering a wider range of evidence about the efforts that GP practices are making to respond to the needs and health inequalities of their practice populations, as well as the outcomes of those efforts, and reviewing how we use this evidence.
- Ensuring that we reflect factors that could disproportionately (although not exclusively) disadvantage ethnic minority-led GP practices in our decision-making processes.
- Reviewing our quality control and assurance processes to consider whether we can do more to remove the risk of any potential bias.
- We will clearly explain our inspection and assessment processes and expectations of all providers so they are easy to understand. To do this:
- We will support all GP practices to understand how to give feedback, challenge our reports and ratings, and raise complaints. This will include reviewing our guidance (including factual accuracy and ratings review processes) to ensure it is clear and accessible to all providers and to inspection teams that support GP practices.
- Inspection teams will continue to build ongoing relationships with GP practices to help them understand our regulatory approach and requirements.
- Carry on implementing our new strategy, so that we work more closely with providers to better understand them and the needs of their populations, and to encourage more open and regular communication.
- Progress our Diversity and Inclusion strategy to increase the number of ethnic minority colleagues at all grades, but especially at senior leadership levels.
- Develop with others our approach to collecting ethnicity data, so we can continue to review how our processes affect practices that are ethnic minority-led.
Introduction
We are the Care Quality Commission (CQC). We monitor, inspect and regulate services, including GP providers, to make sure they meet fundamental standards of quality and safety. We publish findings, including performance ratings, to help people choose care.
We are committed to being a fair regulator that delivers equality in our regulatory approach, driven by people’s needs and experiences and enabling health and care services and local systems to improve.
This report presents the findings of our research carried out in 2021, in response to concerns that practices led by GPs of an ethnic minority background could receive less favourable regulatory outcomes from CQC compared with those led by GPs of a non-ethnic minority background.
We started an initial programme of work in February 2021 to investigate and respond to those concerns and see what further work is needed. This work was conducted at considerable pace to enable us to promptly investigate the concerns raised. Our focus has been on how our own regulatory approach affects ethnic minority-led GP practices and how we can support them in the future.
Background
The quality of care delivered by GP practices in England is generally of a high quality. As at 31 July 2021, of the 6,429 practices on our register that had been rated, 5% (317) were rated as outstanding, 90% (5,806) were rated as good, 4% (276) were rated as requires improvement and 0.5% (30) were rated as inadequate (CQC ratings charts in State of Care 2020/21).
Despite these overall high ratings, we have received concerns from the GP sector about unequal outcomes, particularly for ethnic minority-led practices. These had been discussed in the media and were escalated formally when the Royal College of General Practitioners (RCGP) wrote to us in November 2020 with questions about the impact of our inspections on ethnic minority-led GP practices.
The correspondence highlighted a perception among members of RCGP’s council that ethnic minority-led GP practices received poorer ratings than their non-ethnic minority-led counterparts and were treated less favourably in CQC inspections. The RCGP asked us to work together to ensure transparency and involvement of ethnic minority GPs. At the time the letter was received, we had already started work to explore and review the literature relating to ethnic minority GPs, to understand the context and to help determine the scope of further research.
We are not alone in receiving concerns about differences in regulatory outcomes. Similar concerns have also been raised with other health and care regulators, such as the General Medical Council in Fair to refer? (2019), the Nursing and Midwifery Council’s Ambitious for Change (2020) and the General Pharmaceutical Council’s Managing concerns about pharmacy professionals: our strategy for change 2021-2026 (2021).
Our commitment to reducing health inequalities
The programme of work set out in this report is underpinned by our commitment to helping to reduce inequalities in people’s outcomes from their care and treatment, and to drive improvement for people who need it most.
Our strategy and our Equality Objectives for 2021-25 aim to help deliver equality not only for people who use health and social care services, but also for people working in health and social care, for the health and care providers that we regulate, and for our own workforce. Our ambition is to ensure that our regulation is driven by people’s needs and experiences, and to enable health and care services and local systems to access support to help improve the quality of care.
In our regulation, we expect to see that all people receive the same quality of care, whatever their circumstances. To assess this, we need to consider not only the outcomes for people, but also when a GP practice improves outcomes, for example in areas of deprivation. In this way we will drive improvement to reduce inequalities in outcomes.
The context for this research
We set out to discover the extent of any inequalities in our regulatory outcomes for ethnic minority-led GP practices. As a starting point, we carried out a literature review to understand the context, to help determine the scope, and to develop our research questions.
It is important to note that comprehensive ethnicity data for GPs is not available. For example, the ethnicity of approximately 11% of the GPs on the General Medical Council’s (GMC’s) GP Register is not known. The literature we reviewed has often taken the place of primary medical qualification as a proxy indicator for ethnicity, as this data is readily available – but this has substantial weaknesses, given that many ethnic minority GPs will have received their primary medical qualification in the UK.
Taking this key limitation into account, the literature provides many possible explanations for why there may be a disparity in regulatory outcomes for ethnic minority-led GP practices compared with non-ethnic minority-led GP practices. These include factors that relate to the individual circumstances of GPs from an ethnic minority background and those that relate to their practice environment and the wider system in which they work.
When combined, these factors present as a continuous cycle of inequality (figure 1). Although many of these factors can affect practices led by GPs of all ethnicities, they often disproportionately affect ethnic minority-led GP practices.
Figure 1: The Cycle of Inequality
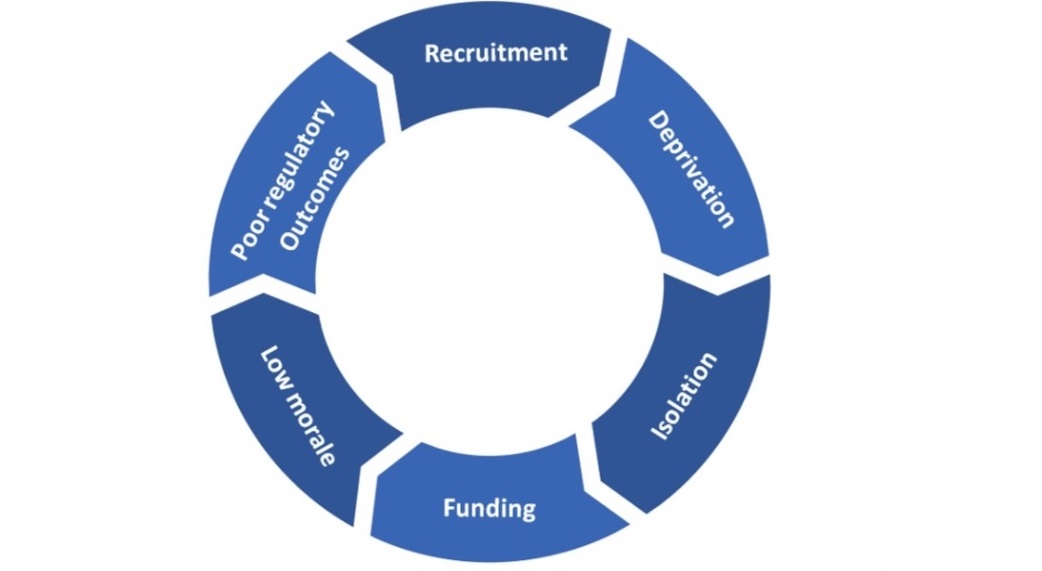
Stigwood, A, 2020
The cycle of inequality starts with recruitment. Literature has previously shown that NHS recruitment processes disproportionately favoured White applicants (The snowy white peaks of the NHS: a survey of discrimination in governance and leadership and the potential impact on patient care in London and England, Kline, 2014), and that inequalities in recruitment continue.
Closely linked to recruitment is the issue of deprivation. Literature has shown that non-UK qualified GPs consistently work in practices in more deprived areas, working with patients who are in poorer health. These GPs are also older and work longer hours (The potential impact of Brexit and immigration policies on the GP workforce in England, Esmail, 2017). The Health Foundation’s briefing Level or not? (Fisher and others, 2020) found that GPs working in areas serving the most deprived patients are responsible for the care of approximately 10% more patients than those located in the most affluent areas. In terms of quality, this briefing also found that practices in deprived areas were more likely to be rated as inadequate or requires improvement.
In the cycle of inequality, after deprivation follows isolation. Non-UK qualified GPs are often recruited into areas of deprivation, where they are more likely to be working in isolation (Esmail, 2017) and operating single-handedly. The General Medical Council’s 2019 report Fair to refer? found that ethnic minority GPs working in professional isolation felt overworked, with little time to promote their own development or that of the wider health system.
Furthermore, the 2020 briefing from the Health Foundation Level or not? (Fisher and others) found that these practices are more likely to receive less funding as, once adjusted for workload, practices in deprived areas receive around 7% less overall funding for each patient (when adjusted for need) than those in more affluent areas.
After funding, the cycle of inequality leads to the morale of GPs from an ethnic minority background. While we did not identify any studies that specifically considered the mental health and morale of these GPs, more general studies have indicated that this could be of concern. The 2019 study GP retention in the UK: a worsening crisis (Owen and others) found that GPs identified complexity of patients, heavy workloads and inadequate funding to be key issues in general practice, which led to stress and exhaustion. These factors often apply disproportionately to non-UK qualified GPs who are more often working in areas of deprivation, which may in turn unduly affect their mental health and morale.
Finally, the cycle comes to regulatory outcomes. These include decisions by regulators about ethnic minority GPs and ethnic minority-led GP providers. In Fair to refer?, the GMC identified that it received a disproportionate number of complaints about non-UK qualified and ethnic minority doctors from their employers compared with non-ethnic minority doctors and doctors who qualified in the UK. This is significant as complaints made by employers are more likely to be investigated. Between 2012 and 2017, employers complained about 1.1% of Black and minority ethnic doctors to the GMC, compared with 0.5% of White doctors.
Literature shows that recruitment can be impeded when practices experience adverse CQC outcomes (CQC inspections: unintended consequences of being placed in special measures, Rendel S, Crawley H, & Ballard T, 2015). Poor regulatory outcomes can deter potential recruits from applying to a particular practice, and the cycle of inequality continues.
What we did
Research questions
The research for this work was based on the overall question:
Does CQC’s approach for regulating general practice have a differential impact on ethnic minority-led GP practices compared with non-ethnic minority-led GP practices? If so, what are the factors associated with these differences and what changes could help to promote equity of CQC’s regulation?
This main question guided our approach. To provide the framework we needed for the work, we split it into three separate parts:
- Is there a difference in ratings, outcomes or experiences between ethnic minority-led GP practices and non-ethnic minority-led GP practices?
- What are the factors that may be associated with differences in ratings, outcomes or experiences?
- What improvement could CQC consider to help promote equity in ratings, outcomes and experiences?
Defining an ethnic minority-led GP practice
As a starting point, we needed to identify practices that are led by GPs from an ethnic minority background. CQC registers and regulates ‘providers’ of GP services. The ‘provider’ may be an individual GP, a partnership of GPs, or an organisation or company. For this work, we excluded parent or corporate companies as we wanted to determine who was providing hands-on leadership at a practice level. We refer to ‘providers’ when we are talking about the legal entity and ‘practices’ when we are discussing the location where the GP services are being delivered.
Identifying ethnic minority-led GP practices presented difficulties for a number of reasons:
- There is no agreed system-wide definition of an ethnic minority-led practice.
- We do not collect data on the ethnicity of the provider and there is no mandatory data collection; this is only collected on a voluntary basis by some other organisations, for example the General Medical Council.
- Some practices may consider their leadership as being wider than the lead GPs or partners.
We consulted with our external stakeholders to develop a definition of an ethnic minority-led GP practice to apply to our research. The agreed definition was:
Where 50% or more of the GP partners are of an ethnic minority background
or
The individual provider or single-handed GP is of an ethnic minority background
To enable us to use this definition, we considered an ethnic minority background to be where a person’s ethnicity is from all ethnic groups except the White British group. (Ethnic minorities therefore include White minorities, such as Gypsy, Roma and Irish Traveller groups.)
We also gave practices the opportunity to self-identify as ethnic minority-led if they felt that they were ethnic minority-led but that our definition did not accurately reflect their leadership.
We carried out a survey of all GP practices (providers) registered with us (6,011). There were 771 responses to the survey, a response rate of 13%. Of the 771 respondents, 51% (390) reported that they met our definition of an ethnic minority-led practice. A further 3% (20) of practices reported that they considered themselves to be ethnic minority-led, but they did not meet our definition. Forty-five per cent of practices responded that they are non-ethnic minority-led (349), with the remaining 12 practices stating, ‘I don’t know’, ‘does not meet definition, practice is part of a company’ or ‘prefer not to say’.
As the majority of practices were able to identify as ethnic-minority-led or non-ethnic minority-led, this gave us assurance in our definition. The 20 practices who considered themselves to be ethnic minority-led but did not meet our definition gave a number of reasons why (figure 2).
Figure 2: Breakdown of reasons why practices did not fit our definition
| Reasons why practices did not meet our definition of ethnic minority-led | Count |
|---|---|
|
We define our practice leadership as being wider than the partners |
7 |
| We define our practice leadership as being only certain partnership members (not all members) | 1 |
| We define our leadership using a different percentage cut-off of partners from an ethnic minority background (less than CQC's definition of 50% of partners being ethnic minority background meaning a practice is ethnic minority-led) | 6 |
| Other | 5 |
| No reason given | 1 |
| Total | 20 |
Methodology
We used a series of quantitative and qualitative methods in this research to answer our research questions. These were targeted both at external stakeholders, GP providers, and internal stakeholders within CQC.
Quantitative methods
Surveys
We designed two surveys: one was to understand the experiences of GP providers, where the focus was on the experience of their most recent inspection of a practice (a number of GP providers have more than one practice location); the other was a survey of our inspectors.
We designed and tested the GP practice survey in consultation with our national professional advisors, subject experts, practising GPs and GP trainees. We sent this to all CQC-registered GP providers (6,011 providers) using the email address that was registered with CQC. The email included a unique link so that we only received one response for each provider. The survey was sent on 6 August and closed on 31 August 2021. We received 771 responses, which is a response rate of 13%.
The survey of CQC inspectors was designed and tested in consultation with the Inspectors’ Reference Group (a group of inspectors who met regularly to discuss the internal CQC elements of this project). We emailed this to all GP inspectors in our Primary Medical Services (PMS) directorate (169 inspectors). A unique link ensured that we only received one response from each inspector. The survey was sent on 31 August and closed on 10 September 2021. We received responses from 57 inspectors, which is a response rate of 34%.
A team of senior analysts and analyst team leaders in our Provider Analytics team and Data Science and Statistics team analysed the data. All the data analyses from the two surveys were quality assured by separate senior analysts and analyst team leaders.
Ethnicity of CQC staff
Electronic staff records hold the personal details of each CQC employee, including self-reported ethnicity data. CQC’s People directorate provided self-reported ethnicity data for a total of 3,129 employees during August 2021. We analysed this data to investigate the diversity at different levels of seniority and within different teams. For CQC’s Primary Medical Services (PMS) directorate, we explored diversity within the GP inspection teams and within the roles that involve making decisions about ratings.
We also reviewed the ethnicity of specialist advisors who provide specialist support for inspections of GP practices, and of bank inspectors who are non-permanent staff engaged with CQC to support inspection work when needed.
CQC’s People directorate provided quality-assured data analysis to the Intelligence teams, suppressing low numbers to ensure people could not be identified.
Qualitative methods
Online community
We commissioned Versiti, an independent research company, to speak to lead GPs from ethnic minority backgrounds about their experiences. We jointly developed discussion guides to use in an online research community, where participants were able to interact with tasks and questions over five days. The aim of the online community was to gain insight into GPs’ lived experiences of CQC regulation, and the results should not be treated as representative for all GPs.
Versiti moderated a five-day online research community of 36 GPs from diverse ethnic minority backgrounds. Of these 36 GPs, 30 self-identified as lead GPs, two did not disclose whether they were lead GPs, and four did not consider themselves to be lead GPs. All participants had experiences of CQC inspections. It was necessary to include these non-lead GPs to ensure that we captured the feedback of a more diverse group of GPs. All the GPs had volunteered to participate in this project. All but one of the GPs had experienced a CQC inspection in the last five years and worked in a mix of urban, suburban and rural areas across England. The sample included male and female lead GPs from a variety of ethnic minority backgrounds (all GP participants identified as being from an ethnic minority background).
The GPs were asked to log in to a controlled website and participate in tasks addressing five overall topics over five days. An online moderator from Versiti posted daily tasks and questions and probed if necessary. Our analysts and the leads for this programme were able to log on and observe the discussions throughout the data collection period and prompt the moderator to follow up on any comments.
Versiti reviewed and structured the data according to themes. They worked with our qualitative analysis team to structure the findings in a report template and produced a report of the qualitative content analysis. Our qualitative analysts reviewed the final report from Versiti to check the clarity and whether the findings were based on evidence from the online community. They shared and discussed feedback with Versiti.
Focus groups and interviews
We used focus groups and interviews to understand the experiences of CQC inspectors, inspection managers and GP specialist advisors. Eight inspectors, four inspection managers and four GP specialist advisors were included. The qualitative analysis team decided on the sample size based on a number of criteria including, but not limited to, the objective for the qualitative research, how large the pool of potential participants was, and how practical it was to recruit a given number of participants in a limited timeframe. The sample size was appropriate for the purpose of this workstream, as the collected evidence was sufficient to address the research question.
We relied on inspectors and inspection managers to volunteer to take part and promoted the work through our internal networking platform and through other staff networks. Specialist advisors received a message through a bulletin, and we emailed 80 specialist advisors who had recently been on an inspection.
We collected data from the focus groups and interviews in August and September 2021, using discussion guides that reflected the research questions. Senior analysts in our qualitative team recorded and transcribed conversations and all discussions were facilitated by either an analyst team leader or a senior analyst.
Our qualitative analysts coded the content of transcripts. The team had regular analytical discussions to report on emerging findings and link findings from different questions into a narrative. This was inductive (data driven) thematic analysis. The team checked the final report to ensure that findings were based on evidence and that it included important findings. Examples and quotes were also checked for accuracy.
Review of our regulatory methods and practice
We reviewed our regulatory methods and how we apply them in practice, to investigate whether there might be opportunities to address any direct conscious or unconscious bias based on ethnicity as well as indirect factors such as deprivation. This work was undertaken by colleagues in our Policy team.
We shared our early findings with senior leaders and decision makers within CQC in a workshop. These senior leaders sit on quality assurance panels to ensure consistency and fairness in our ratings. We held this workshop to give context to how the methodology was developed and to see whether participants could identify any areas within our methodology that could be vulnerable to bias.
Decision making processes
In some instances, for example when a draft report indicates an overall rating of inadequate, that report must be reviewed by a quality assurance panel to confirm the ratings and ensure consistency in decision making.
When we send a draft inspection report to a provider, we ask them to check the factual accuracy and completeness of the information that we used to reach our judgements and ratings.
When we are considering whether enforcement action is required, we hold a management review meeting with inspectors, inspection managers, senior colleagues and experts to decide next steps in terms of regulatory action.
We identified 30 GP practices that met both of the following criteria:
- They had been asked to check the factual accuracy in the draft inspection report.
- We had discussed them at a management review meeting.
It was not necessary for the inspection report to have been through quality assurance panel to be included, but a number of them had.
This meant that we could look across our processes to see how our methods were applied to different GP practices and to compare ethnic minority-led practices with those that were not ethnic minority-led.
We determined whether these practices were likely to meet our definition of ‘ethnic minority-led’. As we anticipated that we would not be able to identify the ethnicity of the practice from data alone, we invited each practice to self-identify.
We contacted 30 practices. Eight practices responded – five practices confirmed that they identified as ethnic minority-led and three confirmed that they identified as non-ethnic minority-led. One further practice informed us that it was in the process of de-registering, so we discarded it from the sample. We do not know the ethnicity of the practices that did not respond. However, if we used the place of primary qualification as a proxy indicator for these practices, 11 additional practices would meet the definition of being ethnic minority-led.
We were unable to classify the remaining practices, which meant that, in total, 16 practices either self-identified as being ethnic minority-led and/or had a majority of partners who qualified outside the UK, and 14 practices did not respond to our request to self-identify or meet the proxy indicator.
We sent 10 of the 30 inspection reports to National Panel (the highest level in CQC’s quality assurance process, which aims to provide an independent objective review of reports and promote consistency in judgements across inspections). Seven out of the 10 reports were for providers that had self-identified as being ethnic minority-led or had a majority of partners who qualified outside the UK.
We reviewed the data to identify any themes that may have indicated issues in how we apply our methods, for example consistency or perceptions around our decision making. We reviewed changes in our guidance and our approach to inspection to understand how they may have affected outcomes or decisions made about practices.
Review of complaints
Our Complaints team reviewed complaints received from NHS GP practices from April 2016 to September 2021 (167 complaints). Each complaint was reviewed to identify any themes specifically relating to bias, discrimination, racism or any other protected equality characteristics. We carried out an in-depth detailed review of five complaints as well as how we responded to them. Of the five complaints, one was upheld, two were partially upheld and two were not upheld, at the time our Complaints team handled them.
Engagement
We wanted our research and findings to be as open and transparent as possible, to make sure we were addressing the important questions that needed to be answered.
At the outset, we publicised our project through our online Citizenlab platform, to explain what we were doing, why we were doing it and our plans to progress the work. We also promoted the GP practice survey through our provider bulletin, and we published internal and external blogs, podcasts and bulletins to keep people informed and tell people how to contact us if they wanted to share their views. We also spoke at CQC’s GP Reference Group, which includes organisations such as primary care networks, NHS Clinical Commissioners and the Digital Healthcare Council.
External advisory group
At the beginning of this programme of work, we identified key representative organisations that were focused on the inequalities faced by GPs from an ethnic minority background. We invited their members to review and comment on our work, from scoping through to fieldwork. These people formed our external advisory group (EAG), who were able to provide expertise and advice as the project progressed and met every month during the project.
System partners
A ‘round table’ of external organisations, regulators and arm’s length bodies – a sub-group of the Primary Care Quality Board – was developed to progress collaborative working across the health system in reducing inequalities faced by ethnic minority-led GPs. The terms of reference for this group are set out in appendix B. The group met monthly throughout the project. The members include organisations with a role in improving the quality of primary care and/or supporting primary care providers and healthcare professionals in England, as well as organisations that represent ethnic minority providers and healthcare professionals.
The initial purpose of this roundtable was to address the concerns in the primary care sector that ethnic minority-led GP practices are more likely to receive lower ratings from CQC and to explore the challenges that ethnic minority-led practices may disproportionately face in meeting their regulatory, legal or commissioning requirements. It has been developed further to progress collaborative working across the health and care sector to reduce inequalities for ethnic minority GPs and also to consider health inequalities.
Inspector's reference group
We developed a reference group of inspectors to support the internal CQC elements of the project, such as the survey of inspectors and our review of regulatory methods. We asked for volunteers through our staff bulletin and by email, and held regular meetings to gather feedback and support during the fieldwork stage. This was to ensure that we captured the expertise and experience from a wide range of inspection colleagues.
Subject matter experts
To help develop our methods and research questions for this programme of work, we consulted with experts in the field of inequalities in primary care, asking for their advice and support and updating them with our findings.
What we found
Research question 1: Is there a difference in ratings, outcomes or experiences between ethnic minority-led GP practices and non-ethnic minority-led GP practices?
To answer this question, we considered the following:
- Statistical modelling, to understand whether there is an association between the ethnicity of doctors working in a practice and CQC ratings after taking into account other factors that can be associated with ratings (for example, deprivation in the local area).
- Accounts from ethnic minority GPs, shared in the online research community.
- Results from the GP practice survey – in particular, any notable differences in the results from ethnic minority-led and non-ethnic minority-led GP practices.
- Views of CQC inspection teams, shared in interviews and forums and from the results of the inspector survey.
We have split our findings into several sub-questions.
Do ethnic minority-led practices have poorer ratings?
To establish whether there is a difference in our ratings of ethnic minority-led and non-ethnic minority-led GP practices after accounting for other factors that could affect ratings, we hoped to perform statistical modelling using data held by CQC about GP practices and their local area, and national indicators, as well as data held by the General Medical Council (GMC) about the demographics of registrant GPs.
However, the data that were available were not sufficiently complete to perform effective statistical modelling that would ensure that any conclusions were robust and based on good evidence.
Challenges included a lack of full ethnicity data for the majority of GP practices and not being able to match some GMC data to CQC-registered locations. This left a small sample size of around 20% of all rated GP practices (1,324) with full ethnicity data (this is 20% of all GP practices, rather than GP providers as some providers run more than one practice). In addition, the number of GP practices that were rated overall as requires improvement or inadequate was low (100 practices), making it unlikely that a model would be able to detect a relationship between the ethnicity of doctors working in a practice (or other factors) and ratings, even if such a relationship existed.
We also lacked consistent historical data for key variables, such as the health profile of the patient population, due to changes in data collection for the NHS GP Patient Survey in 2018. This meant we would have had low confidence in the results of the model. For example, if we found a relationship between the ethnicity of doctors and our ratings, we would not be able to rule out that this was because practices with a high proportion of ethnic minority doctors serve populations with a higher prevalence of long-term health conditions. For this reason, we were unable to fully answer the first part of this research question. See appendix A for more details of the statistical model.
In our GP inspector survey, we asked whether there were perceptions of difference in ratings:
- 37% (20/54) of inspectors disagreed that ethnic minority-led practices were more likely to have poorer ratings
- 37% (20/54) gave a neutral response
- 26% (14/54) agreed.
This highlights that the majority of inspectors either did not perceive there to be a difference in ratings between ethnic minority-led and non-ethnic minority-led practices or had no opinion.
However, the perceptions of inspectors were not echoed by ethnic minority-led GP providers. In the GP practice survey, ethnic minority-led GP providers perceived that they had a poorer inspection outcome based on their ethnicity: 31% (124/400) of ethnic minority-led practices agreed or strongly agreed that their inspection outcome was adversely affected by ethnicity, compared with only 0.3% (1/304) of non-ethnic minority-led practices. (Note: A small number of ethnic minority and non-ethnic minority respondents answered ‘not applicable’ for these survey questions and were removed from the denominators.)
Are ethnic minority-led practices more likely to be inspected?
As we could not complete statistical analysis, we were unable to report whether ethnic minority-led practices were more likely to be inspected. However, we did ask for views that are relevant for this question.
In our survey of inspectors, we asked them to rank the top three factors that were most likely to trigger an inspection outside of planned inspection frequencies for all GP practices (which were based on ratings). These were:
- whistleblowing concerns 51% (29/57)
- information of concern raised by the CCG 16% (9/57)
- deterioration in performance of key indicators (QOF, GP Patient Survey, Public Health) 14% (8/57).
Fifty-seven per cent (31/54) of inspectors disagreed that ethnic minority-led practices were more likely to have an inspection triggered by information of concern, although 13% (7/54) agreed and 30% (16/54) gave a neutral response.
Similarly, one inspection manager mentioned in a focus group that they could not think of anything specific that would single out ethnic minority-led GP practices. Rather, they explained that the frequency of inspections was based on previous ratings, risk, data and other information of concern.
Through the GP practice survey, we asked whether the most recent inspection was carried out through an on-site visit or completed off-site.
On-site inspection visits were carried out for:
- 61% (251/410) of ethnic minority-led practices
- 69% (242/349) of non-ethnic minority-led practices
The proportion of inspections that were completed off-site was almost the same for both:
- 26% (108/410) of ethnic minority-led practices
- 27% (93/349) of non-ethnic minority-led practices.
There was a bigger difference in inspections that were a mixture of on and off-site, although the numbers are small:
- 12% (49/410) of ethnic minority-led practices
- 3% (12/349) of non-ethnic minority-led practices.
This implies that there is no notable difference in the types of inspections CQC uses for ethnic minority-led and non-ethnic minority-led practices.
We usually visit practices with poorer ratings or where we are taking enforcement action more frequently than those rated as good or outstanding. We do not know definitively whether ethnic minority-led practices do indeed receive poorer regulatory outcomes. However, if we assume that ethnic minority-led practices are more likely to experience certain contextual factors (discussed under the headings of ‘external system factors’ and ‘internal practice factors’ in this report), which may be associated with poorer inspection outcomes, then it is conceivable that there is a perception of more frequent inspection. However, it is important to note that this is merely a hypothesis and further research would be needed to explore this issue further.
Do ethnic minority-led practices have a differential experience of the inspection process and outcomes?
Through our research, we heard about GPs’ experiences of our inspection process and outcomes in two ways:
- through the GP practice survey (targeted at all GP practices)
- through the online research community (which engaged only GPs from ethnic minority backgrounds).
Therefore, the findings from the online research community only reflect the lived experiences of ethnic minority GPs, and direct comparisons with White British GPs are not appropriate.
Online research community findings
The online research community consisted of 36 GPs from ethnic minority backgrounds. This found that many experienced CQC inspections as a ‘threat’ and a punitive process rather than an opportunity to review, learn and grow. Moreover, many of these GPs reported feeling panicked and anxious in anticipation of a CQC inspection and that the inspection itself felt intrusive.
When ethnic minority GPs in the online research community were asked about the outcomes of inspection, they felt their results were usually in line with their own expectations, but the outcomes of the inspections rarely added value to the work of the practice.
Some GPs participating in the online research community felt that the inspection outcomes were ‘harsh’ and ‘unfair’ and did not consider the realities faced by the practices and their populations.

“My biggest ‘headache’ is probably CQC and the threat of an inspection because my mind is drawn to one particular CQC inspection in which I thought we would do really well and we would get outstanding. However, we were grilled for almost 10 to 12 hours [...] and despite getting good, we were still criticised for bowel screening figures which I felt was unfair as we have no control over bowel screening.”
(Male, Pakistani, Midlands)
The majority of the GPs who participated in the online research community had concerns around racial discrimination leading to unfair treatment from regulators, including CQC. A consistent theme among most of the participants was a sense that regulators do not understand or appreciate the challenges that ethnic minority doctors face. Some felt that assumptions are made about what an ethnic minority-led practice is like, seeking information to confirm their low expectations and ignoring positive evidence, resulting in a ‘predetermined outcome’.

“Whenever anyone comes to see us from NHSE/CQC/CCG, I always get the impression they make a judgement on us based perhaps on many reasons. Demographics, our names, our population, our location perhaps? But that judgement/stereotype is usually changed once they talk to us. It always helps I feel to have an English accent.”
(Male, Pakistani, North West England)
GP practice survey findings
In the GP practice survey, we were able to identify some key differences in the reported experiences of ethnic minority-led practices and non-ethnic minority-led practices. These were:
- 38% (156/410) of ethnic minority-led practices, compared with 26% (92/349) of non-ethnic minority-led practices, reported that one or more GPs in their practice experienced an adverse impact on their mental health because of the inspection process. Response rates were similar when comparing practices that served in areas of deprivation with those that did not (35% (133/383) and 31% (116/373) respectively).
- 51% (210/410) of those who identified as ethnic minority-led, compared with 41% (142/349) of non-ethnic minority-led practices, experienced a negative impact on their personal and/or family life because of the inspection process. We found similar results in practices that served a socio-economically deprived population (47% or 181/383 were negatively affected). However, this is similar to practices serving predominately non-deprived areas, where 46% (171/373) were negatively affected.
- 23% (93/410) of respondents from ethnic minority-led practices, compared with 7% (24/349) of respondents from non-ethnic minority-led practices, reported adverse physical health problems because of the inspection process. Practices serving predominately socio-economically deprived populations were almost twice as likely to report experiencing adverse physical health problems because of the inspection process compared with those in non-deprived areas.
- 23% (93/410) of ethnic minority-led practices, compared with 7% (23/349) of non-ethnic minority-led practices, felt that there had been an increase in staff sickness because of the inspection process.
- When comparing practices, 52% (212/405) of ethnic minority-led practices agreed or strongly agreed that the final inspection report and rating accurately reflected their practice, compared with 65% (226/346) of non-ethnic minority led practices. A higher proportion of ethnic minority-led practices than non-ethnic minority led practices disagreed or strongly disagreed with the statement (31% (124/405) compared with 17% (60/346).
- 27% (109/410) of ethnic minority-led practices, compared with 14% (48/349) of non-ethnic minority-led practices, agreed or strongly agreed that patient care improved following inspection. Almost half of respondents (360/771) neither agreed nor disagreed that inspections improved the quality of patient care.
The view of CQC inspection teams
We spoke to CQC inspectors and inspection managers, and GP specialist advisors to ask them about their perceptions and experiences of inspecting and regulating ethnic minority-led GP practices. They emphasised that they felt the ethnicity of the provider did not play a direct role in their approach to inspection or regulation; we discuss this further in research questions 2 and 3.
Some CQC colleagues gave examples of where differences between the approaches of inspection teams could have led to different outcomes. We heard from a specialist advisor who said they thought some inspectors might go into a practice with preconceptions which, as a specialist advisor, were difficult for them to challenge. This aligned with some views expressed by ethnic minority GPs in the online research community, that some CQC inspectors may have predetermined views.
There were also positive examples of specialist advisors and inspectors supporting GP practices to give the right evidence, for example by rephrasing questions, asking for evidence differently and spending more time finding the right evidence.
These findings suggest that there is a potential for different outcomes and experiences across our inspection process. We discuss in further detail the potential factors contributing to these differences in research question 2.
Recap
Due to limitations in the data available to us from all partners in the system, we were unable to fully explore the nature of the relationship, or existence of any causal link, between ethnic minority-led GP practices and regulatory outcomes such as ratings and frequency of inspection.
The majority of CQC inspectors did not agree that ethnic minority-led practices were more likely to have an inspection triggered by information of concern. In the focus groups with inspection teams, some inspectors and inspection managers linked the frequency of inspections to a practice’s performance, for example if they were in special measures, and emphasised that the inspection methodology is based on risk. The GP practice survey also indicated that there is not a notable difference in the types of inspections CQC uses for ethnic minority-led and non-ethnic minority-led practices.
However, ethnic minority GPs’ experiences of CQC’s inspection process and outcomes appear to be poor. We heard in the online research community that ethnic minority GPs felt inspection outcomes can be “harsh” and “unfair”. Most also had concerns about racial discrimination in regulation leading to unfair treatment, and felt that CQC, among others, does not understand or appreciate the unique challenges that ethnic minority doctors face. Some felt that assumptions are made about what an ethnic minority-led practice is like, leading to inspectors seeking information to confirm their low expectations and ignore positive evidence, resulting in a “predetermined outcome”.
In the focus groups with inspection teams, inspection colleagues told us that many ethnic minority-led practices that they had inspected had been in special measures. This could possibly lead to an impression that ethnic minority-led practices are inspected more frequently overall. Practices in special measures are inspected more frequently than those with a rating of good, to ensure that risks are mitigated. This association of ethnic minority-led practices with practices in special measures may create some unconscious biases towards these types of practices.
While we were unable to compare these experiences against those of non-ethnic minority GPs, the GP practice survey highlighted that ethnic minority-led practices were more likely to report that GPs in their practice experienced adverse impacts on their physical and mental health, personal and/or family life, and that they had seen an increase in staff sickness as a result of the inspection process. Ethnic minority-led practices were more likely to report that they agreed or strongly agreed that their inspection outcome was adversely affected by ethnicity compared with non-ethnic minority-led practices. A higher proportion of ethnic minority-led practices than non-ethnic minority-led practices disagreed or strongly disagreed that the final inspection report and rating accurately reflected their practice.
However, the GP practice survey highlighted some positive impacts, namely that ethnic minority-led practices were more likely to report that quality of care improved following a CQC inspection.
Research question 2: What are the factors that may be associated with differences in ratings, outcomes or experiences?
In this section, we present our findings in relation to the factors that may influence inspection outcomes. These include ‘internal factors’ that are internal to the practice such as its characteristics and leadership, ‘external factors’ that relate to the wider healthcare system and ‘internal CQC factors’ that relate to CQC’s processes and methodology.
Factors internal to ethnic minority-led practices
We know from our literature review that non-UK qualified GPs tend to work in practices in higher areas of deprivation, where patients are in poorer health. GPs in these practices are responsible for more patients and more likely to be working in isolation or operating single-handedly. Many of these factors can contribute to differences in ratings, outcomes or experiences of CQC regulation.
Single-handed or individually led practices:
In our survey of GP practices, 19% (143/771) of respondents stated that their practice was single-handed or individually led at their most recent inspection. Of these, 85% (121/143) stated that their practice was ethnic minority-led.
We know from feedback received in the online community of ethnic minority GPs that inspections were perceived as especially problematic and burdensome for smaller practices that had reduced capacity to focus on regulatory compliance.

“It is a stressful, bureaucratic, draconian nightmare which is designed generically but doesn’t take into account the size of an organisation. It is difficult, challenging and unrealistic. It also is very time consuming and sometimes pedantic… Some of the [key questions] apply to large organisations, and [a] small GP practice with five staff would simply struggle to be able to comply.” (Male, Indian, London)
In our internal focus group and interviews with CQC inspectors, inspection managers and specialist advisors, several participants emphasised the challenge associated with small and single-handed GP practices. This was perceived as frequently disadvantaging ethnic minority-led GP practices. It was discussed that single-handed practices were more often professionally isolated, while also having limited time to undertake inspection-related activities.

“It's often smaller practices that are already suffering, quite isolated, already struggling to attend all the meetings in their CCGs and they are often very isolated.”
(CQC specialist advisor)

“[…] with the amount of reporting and stuff that they've got to do, single handers often struggle with the reporting of things, even if they have actually done them.”
(CQC inspector)
Therefore, although we found that respondents in the GP practice survey who identified as ethnic minority-led were more likely to be rated as requires improvement or inadequate (51/59 requires improvement, 8/9 inadequate were ethnic minority-led), this may reflect the higher proportion of single-handed ethnic minority-led practices that responded to our survey and the challenges associated with our inspection methodology for these types of practices.
Practice management and leadership:
Participants in the internal CQC focus group and interviews discussed several factors related to poor practice management or leadership, which could affect inspection outcomes. Many of these were associated with single-handed practices, which the literature and survey findings suggest may be disproportionately ethnic minority-led.
CQC’s management review meetings are meetings to consider and discuss next steps when risk is identified. In the review of 30 management review meetings, we found that seven were held owing to concerns with leadership. All seven of those practices were among those that had self-identified as being ethnic minority-led or had a majority of partners who qualified outside the UK.
One inspector noted that, in their experience, many single-handed practices were run by GPs who qualified before CQC began regulating the sector. Several CQC colleagues thought that some GPs may face challenges in achieving good inspection outcomes as they had spent much of their working life without CQC regulation. In comparison, the participants felt that more recently qualified GPs may be more aware of, and have a greater understanding of, the expectations of today’s primary care, including the expectations of CQC regulation.

“A lot of the single-handed GPs that we have, and [who] I've met on inspection, a lot of them would have been […] older GP[s] and I think that the demands of modern primary care are certainly very different to those when they started off.”
(CQC inspector)
Some focus group and interview participants discussed IT skills as an important factor associated with inspection outcomes. As one specialist advisor emphasised, a GP’s ability to access and present relevant data and evidence can potentially affect the inspection process.

“I think IT plays a big role as well because perhaps some of the doctors are older and less tech savvy and everything is based on IT. Even to the extent of our new modus operandum, we’re doing all the Teams calls, and if you're not very good with Teams then you can't present the evidence or present yourself as well as you need to. A lot of things might be on paper or might be there but are not done. But unless everything is organised in an IT way then it's difficult.”
(CQC specialist advisor)
A few participants in the focus groups discussed that a GP’s inability to provide evidence within the inspection was associated with poorer inspection outcomes even if the practice fulfilled their regulatory obligations. As one inspector explained, impressions regarding competence and management could be formed by the inspector where necessary evidence was not provided within the inspection. Single-handed GP practices were more often associated with the challenge of presenting information and evidence. One inspector noted that the inability to provide information and evidence within the inspection could not be excused.

“So, what I tend to see is that there are gaps in the evidence, and I think that comes back to [the] challenge [of demonstrating] the evidence. In all possibility, they are actually complying, but they don't have the time, they don't have the hands on deck to be able to prove their evidence. And that's not acceptable as an excuse for us.”
(CQC inspector)
Several participants in the focus groups and interviews discussed family members as often being involved with the running of single-handed ethnic minority-led practices. Family-run practices were found to be a further factor associated with inspection outcomes, where there was limited training in place for family members, meaning a practice may not be managed and monitored effectively.
Other challenges were found to be associated with family-run practices. For instance, we heard from some focus group participants that the established methods of working, and the close family connection of family-run practices, made it more challenging for inspectors to engage with the practice and make suggestions to support the practice where possible. However, examples were given of how family relationships can have a positive impact on inspection outcomes. We heard one example of how a family member joined a practice’s leadership team and was able to drive change and work with a CQC team to improve the services provided.
Participants emphasised that challenges associated with family-run practices might disproportionately affect ethnic minority-led providers. However, they did not think that ethnicity itself had an impact on inspection outcomes. Participants considered the issues associated with poor practice management and leadership as potentially affecting inspection outcomes.
It is important to highlight that these were the views of CQC inspection teams. Therefore, while these findings highlight some internal challenges for ethnic minority-led practices, they also shed light on some potentially preconceived ideas or unconscious biases about particular types of practices, which might disadvantage ethnic minority-led practices.
Factors external to ethnic minority-led practices
As discussed in the previous section, ethnic minority-led GP practices often work in environments that may pose additional challenges. In this section, we explore the relationship between the wider healthcare environment, the GP practice and CQC regulation.
Ethnic minority communities and levels of deprivation:
Most GPs from ethnic minority-led practices that we spoke to in the online research community said that they operated in areas with a high concentration of people from ethnic minority communities and with high levels of deprivation. They consistently reported challenges that they felt were different from, or more acute than, the national profile. GPs who participated highlighted that ethnic minority-led practices often struggled with patients with complex long-term health needs, such as cancer, diabetes, heart disease and mental ill-health. They also mentioned challenges of low staffing levels, barriers to accessing care, and being over-subscribed to deliver care.

“We have a much younger population compared to the CCG and nationally, and […] the majority of these patients have English as a second language. Our CCG as a whole has the second highest proportion nationally of [Black and Ethnic Minority] patients (I think). Our population is much more deprived with some of the highest incidences of [Serious Mental Illness], together with double the national prevalence of type 2 diabetes. A large proportion of our newly registered patients have only recently arrived in the UK, mainly from Romania, Afghanistan, Iraq and Iran. These patients have massively complex needs – either due to the patients not having access to healthcare for many years, mental health and physical health issues as a result of their traumatic experiences, poverty and different health beliefs due to cultural factors.”
(Male, Indian, London)
In our survey of GP practices, 65% (267/410) of practices that identified as ethnic minority-led stated that they served a socio-economically deprived population, compared with 32% (113/349) of non-ethnic minority-led practices.
We asked practices whether CQC reflected their challenging factors in their inspection and/or rating. A larger proportion of ethnic minority-led practices than non-ethnic minority-led practices found the socio-economic deprivation of the practice’s population to be a challenging factor. Of all the respondents, 45% did not feel that their most challenging factor was reflected in their inspection/rating. For ethnic minority-led practices, this proportion was 52% (199/382), whereas for non-ethnic minority-led practices it was 38% (119/314). Note: respondents who answered ‘don’t know’ were removed from the analysis.
In our survey of CQC inspectors, the 57 respondents identified the top three factors most likely to pose a challenge to all GP practices as: socio-economic deprivation, low GP-to-patient ratio, and geographical considerations (figure 3). When discussed further in focus groups and interviews, colleagues noted that socio-economic deprivation levels within patient communities influenced the ability of GPs to achieve national targets considered by CQC.

“It's complicated because you can't just say all ethnic-background providers work in deprived areas, because that's not true. But, with practices in areas with high levels of deprivation, and I wouldn't at all equate these with being led by ethnic minority background GPs, but often they are […] they have very different patient populations with challenges […] they will never achieve the kind of percentages on monitoring data stats that we look at. They can try as hard as they like.”
(CQC inspector)
Figure 3: Comparison of responses between respondents in the GP practice survey and CQC inspector survey: What are the top five challenges faced by GP practices?
| GP practice survey: Responses from ethnic minority-led practices | Inspector survey: Overall results | |
|---|---|---|
| Challenge 1 | Patient expectations that cannot be met due to constraints | Socio-economic deprivation of the practice’s population |
| Challenge 2 | Complexity of patients’ health and communication needs | Low GP-to-patient ratio |
| Challenge 3 | Socio-economic deprivation of the practice's population | Geographical considerations (inner-city, remote, coastal, rural etc) |
| Challenge 4 | Direct effects of the COVID-19 pandemic on provision of care |
Complexity of patients’ health and communication needs Inadequate funding Professional isolation Recruitment and/or retention of GPs |
| Challenge 5 | Inadequate funding | Direct effects of the COVID-19 pandemic on the provision of care |
In focus groups, some inspectors and specialist advisors strongly noted that there was limited recognition within CQC’s methodology, including quality assurance panels, of the disadvantage of the surrounding contexts in which these practices exist. Rather, these participants emphasised that CQC’s inspection methodology does not sufficiently consider surrounding contexts, noting this as a challenge to achieving good inspection outcomes and discussing practices as being penalised for not achieving similar outcomes to practices with very different contexts and patient communities.

“I think deprivation is an important factor. It's really not taken into account in any way, shape or form, and the great difficulties that have to be undertaken due to that, and it's just assumed that all the outcomes will be perfectly as good as other areas.”
(CQC specialist advisor)
One inspector did note that while deprivation may be a negative factor to some practices’ inspection outcomes, they had had experience of inspecting flourishing practices within similar contexts.

“You know, I've also been to some practices where they've been in a high deprivation area, but actually been achieving well, so it's not always the case.”
(CQC inspector)
Workload and recruitment of staff:
We know that patients in areas of high deprivation tend to have poorer health and more complex needs. Often, these patients need more care from GPs.
Most of the GPs in our online research community highlighted an increase in demand for their services, especially in relation to COVID-19 and delays in secondary care. GPs felt that this was expected of them without any improvement in resourcing. This was further exacerbated by challenges in recruiting and retaining staff, particularly in practices that were working in areas of deprivation with large proportions of patients who were from ethnic minority backgrounds.

“Recruitment has always been difficult. As we are on the fringes of a city, rarely get more than one applicant when we advertise for doctors or clinical staff. In terms of admin staff, there has been a large turnaround of staff in the recent past. Many have left due to the attitude of patients towards them. [...] We have been short 1.5 full time equivalent GP for 2 years but having problems recruiting. The practice has hired paramedics and pharmacist to help with workload but we are short on doctor appointments.”
(Female, Arab, London)
Literature shows that recruitment may be impeded when practices experience adverse CQC outcomes (Rendel S, Crawley H, & Ballard T 2015). In our GP practice survey, we asked whether a CQC inspection had resulted in additional staff being recruited. Those that reported that staff were recruited after a CQC inspection were more likely to be ethnic minority-led. Ethnic minority-led practices were also more likely to experience challenges in recruiting staff. It is therefore difficult to understand whether these problems arise as a result of inspection activity or are pre-existing problems that are exacerbated by poorer ratings.
Additionally, some inspectors in our focus groups and interviews highlighted the impact of funding and investment as posing a challenge to recruitment. They discussed how single-handed practices often struggle to recruit enough clinical staff owing to their limited funding, and perceived single-handed practices as often not having enough staff to support practice demands. It was noted that this was compounded by practice staff often moving from single-handed practices to larger practices because of the greater training and development opportunities that larger practices could offer.

“It’s really difficult to get a good practice nurse […] there isn’t enough money to pay staff, and when you’re in a single-handed practice like that, there’s less money to pay staff to go do courses, to make sure their training is kept up to speed.”
(CQC Inspector)
Support from system bodies:
Support from external bodies within the health and care system can be helpful for GP practices in overcoming challenges and delivering high-quality care for all. However, we heard in the online research community that practices led by ethnic minority doctors often lacked leadership support from other bodies and suffered from low morale. Discussions with our CQC colleagues noted that support from the system, for example through CCGs and primary care networks (PCNs), varied between areas and often favoured larger practices and overlooked smaller single-handed practices.

“It may have an impact on regulation, but I think a lot [of] focus is on those big groups of GP practices who are […] high up in the PCN. Perhaps a smaller, sole provider gets lost or gets left behind. Although […] the onus is [actually] on the PCN to not leave them behind but specifically to put in support to make sure that they are coming up to regulatory standards.”
(CQC inspector)
This was echoed by ethnic minority GPs in our online community and, importantly, we heard an example from an inspector that GP ethnicity had an impact on the level of support received by practices.
Despite the likely benefits that system support would bring to practices that needed to make improvements, many respondents to the GP survey felt that there was no improvement in engagement with external bodies following an inspection, although this was not related to ethnicity. In our online community, ethnic minority GPs told us about their experiences.

“At times I feel I am really isolated and have to deal with several issues in isolation. We need more support from the CCG in terms of training and funding.”
(Female, Indian, North West)

“Since I relocated to the UK […], I have constantly experienced racism both direct and institutional. [outlines an instance of bullying and harassment by a member of practice staff] This issue was raised during CQC inspection. The advice was to ‘forget about it’ and move on. I was expecting the CQC to make a recommendation to NHSE.”
(Female, Black, North East)
However, CQC colleagues also noted that, occasionally, ethnic minority-led practices may sometimes be reluctant to engage with support from system partners because of a mistrust of other bodies.

“I also think there may have been an element of some of the GPs thinking that the CCGs are interfering, and so perhaps it wasn't necessarily the CCGs always not helping; sometimes they were a little bit insular themselves.”
(CQC inspector)
Funding and investment:
Both our online community of ethnic minority GPs and CQC colleagues reported that funding and investment can pose a problem for ethnic minority-led practices. Some CQC colleagues reflected that this may be linked to working in more deprived areas.

“[I]f you have a high level of deprivation and you're trying to eke your funding out amongst everyone, you don't have time for the social niceties and those things that are really going to raise you above the bar, because you're struggling to actually provide a decent basic level of care.”
(CQC inspector)
While CQC is not responsible for funding, nor do we rate providers with an expectation that this will have an impact on funding, engagement during this work indicated concerns that funding issues may be worsened by poor inspection ratings and that this can have a consequential impact on performance and therefore future regulatory outcomes. Funding can also show how the wider system is responding to providers’ performance, which we reflect on in more detail under the next research question.
We asked practices to indicate whether they agreed with a statement saying that funding increased following their CQC inspection. Many respondents to our GP practice survey (79%, 610/771) reported that, following a CQC inspection, there was no increase in funding, irrespective of ethnicity.
We also looked at the responses to this question against ratings. Seventy-two per cent (28/39) of practices rated as outstanding disagreed or strongly disagreed that funding increased following their CQC inspection. Of practices rated as good, 78% (507/651) also disagreed or strongly disagreed, as did 97% (57/59) of practices rated as requires improvement and 78% (7/9) of those rated as inadequate. It therefore appears that most practices, regardless of their rating, felt that funding did not increase following a CQC inspection.
When we looked at the data by deprivation, there was virtually no difference in responses about funding, regardless of whether or not practices considered their populations to be socio-economically deprived. Eighty per cent (307/383) of practices in deprived areas disagreed or strongly disagreed that funding increased as a result of the inspection, 18% (68/383) neither agreed nor disagreed and 2% (8/383) agreed or strongly agreed. For practices in non-deprived areas, 78% (292/373) disagreed or strongly disagreed that funding increased, 19% (72/373) neither agreed or disagreed and 2% (9/373) agreed or strongly agreed.
In the GP practice survey, 67% (514/771) of respondents disagreed or strongly disagreed that there was support for service expansion following their inspection; 72% (554/771) disagreed or strongly disagreed that there was support for additional training or teaching.
Within the focus groups, CQC colleagues discussed a practice’s funding and investment as important to achieving good inspection outcomes. However, the inspectors did not specifically relate this association between funding and investment to ethnic minority-led practices. One inspector discussed that a practice’s ability to provide outstanding services was closely tied to their access to funding and investment.

“Where you've got outstanding practice […] or outstanding features, it's likely to be because they have access to funding, or to additional funding for whatever reason, which gives them that ability to offer a service of above and beyond.”
CQC inspector)
Interactions with patients:
The interactions between ethnic minority-led GP practices and patients have also featured as potential causes for differential experiences and outcomes in CQC ratings. As we have examined from the GP practice survey, the socio-economic deprivation levels within a population and the complexity of patients’ health needs can present significant challenges to GP practices. However, the interaction with patients themselves and the difficulties in meeting expectations when practices are under pressure can have implications on patient satisfaction and complaints, and therefore inspection triggers and outcomes.
When we spoke to ethnic minority GPs in our online community, they told us that patient expectations had been rising over time, which against a background of inadequate funding or funding cuts by CCGs made it more challenging to deliver care. Some ethnic minority GP leads told us that they had experienced racism from patients, especially when those patients’ expectations could not be met. In some cases, patients had refused to see GPs of an ethnic minority background.

“I have had Caucasian patients directly refusing to be consulted by me due to my skin colour and for being of Asian origin. I felt supported by my colleagues when this has happened. On one occasion all my colleagues declined to see the patient as a show of support. I have also found that patients are more likely to complain about a 'non-White' clinician.”
(Male, Indian, North West)
GPs we spoke to also felt that patients were more likely to complain about ethnic minority GPs than White British GPs. It can be difficult for CQC to discern whether the concerns we receive are racially motivated or biased, unless the complainant is overtly racist in their complaint. In our review of 30 management review meetings, which are convened to discuss further action when risks are identified with a practice, two of these were convened as a result of, either wholly or partially, a patient complaint. One of these practices identified as ethnic minority-led and the other was led by partners who qualified outside the UK. However, from this small sample it is difficult to draw conclusions about the motivation for complaints. Although we heard that there had been fewer racist incidents in recent years, we are aware that evidence from other pieces of work, flagged by our External Advisory Group, have found the opposite and that racist incidents have increased in some areas.
Similar themes were identified in our discussions with CQC inspectors, inspection managers and specialist advisors. It was perceived that negative feedback and complaints made about ethnic minority GPs were often triggered by patient expectations and satisfaction, with GP communication being highlighted as a prominent issue. Communication between GPs and their patients is important, but some complaints could be made against ethnic minority GPs owing to societal racism and biases.

“I think for me, it's a consideration, you know, where someone has clearly said within an inspection, we are subject to people making racist comments about us. That, for me, it has to be consideration. But currently, I don't feel that we really have the ability to reflect that in an inspection report very well.”
(CQC Inspector)
Internal CQC factors
CQC’s core purpose is to make sure health and social care services provide people with safe, effective, compassionate, high-quality care and to encourage care services to improve. While feedback from inspectors demonstrated commitment to our core purpose in respect of standards of care, our findings indicated that we may not always consider all relevant factors in our inspection approach to enable us to effectively encourage improvement.
Striving for objectivity:
Inspection colleagues said that during inspections they strive for objectivity and consistency, and they referred to inspection outcomes as being based on evidence. Several inspectors and inspection managers referenced the inspection guidance documents, including the inspection framework, decision trees and quality assurance processes, which they thought ensured that any judgements were based on fact rather than opinion, thereby ensuring consistency.
Inspection colleagues emphasised that their key priority was ensuring that care was safe and accessible, regardless of the challenging circumstances that practices might face. Colleagues said that, while they acknowledged that some data might be poorer for some practices owing to external challenges, they expect providers to adhere to certain standards.

“You are going in without fear or favour because you’re following a framework methodology and you are there to make sure that practice is safe. [….] There wouldn't be any difference in how we measure what safe, effective and well-led practices are, because the methodology wouldn't allow for it. I would hate for us to start to think that we're doing things differently, because I can honestly say having done numerous such inspections we are not.”
(CQC Inspector)

“The regulations are the regulations. We instil those regulations for everybody. And when registering with CQC, it is their responsibility to follow the regulations.”
(CQC inspection manager)
However, ethnic minority GPs in the online community expressed their concern that CQC’s inspection processes and methodology do not allow for specific challenges or needs to be taken into account, and that this can lead to poorer inspection outcomes. Through discussions with our online research community, it emerged that, by applying a universal, identical methodology to all GP practices in pursuit of consistency, CQC may unwittingly produce inequities that lead to unfair outcomes where the methodology is not sufficiently tailored to reflect providers’ circumstances.
Many inspection colleagues felt there was no difference between regulating ethnic minority-led and non-ethnic minority-led practices. In discussions, we heard that there were some perceptions that linked certain characteristics with ethnic minority-led practices, such as deprivation and operating single-handedly.
In addition, some felt that the way evidence, in particular data, is considered in the inspection process could be perceived to disadvantage some ethnic minority-led practices that might be more likely to work in challenging circumstances.
Inspection colleagues in the interviews and focus groups described how input from inspectors is often the balancing factor for practices whose data and performance measures are affected by socio-cultural factors, such as deprivation and multiple cultures. The extra effort that inspectors and specialist advisors take to drill down during inspections, and in requesting data from GPs, is instrumental in helping these GPs and their practices meet requirements that influence their inspection outcomes. Inspection managers indicated how members of their inspection teams must work harder to get information from GP practices in areas of deprivation and multi-ethnicity, and by doing so, obtain information that can help mitigate against poor ratings.
Make-up of inspection teams:
In the online research community, GPs from an ethnic minority background raised concerns about the ability of some CQC inspection teams to support ethnic minority-led GP practices. They told us that they would feel more reassured if CQC inspectors could demonstrate greater cultural competence.
There were some views that a better understanding of a GP’s background and experiences could lead to a more supportive relationship between CQC and practices. This included reflecting on what GPs have experienced and how they are feeling, as well as developing greater cultural competence. GPs in the online community also told us of their impression that inspectors were middle class and of a White ethnicity, which could mean that they lacked the diversity and understanding of the specific health needs of the diverse populations which they served.

“CQC and its inspectors need to show an understanding of the diversity and cultural aspect of ethnic minority-led GP practices and the population it serves.”
(Male, Black, East of England)
Labour market data shows that 13% of the workforce in the UK are from ethnic minority groups. However, the GMC’s GP register tells us that of 79,630 GPs on its register, 59% are of a White ethnic background, 28% of an ethnic minority background, 2% prefer not to say and 11% are not known. Within GP inspection teams in CQC’s Primary Medical Services (PMS) directorate, 21% of inspectors (46/216) and 17% of inspection managers (8/48) identify as being part of an ethnic minority group. Among the senior roles within the PMS directorate, 13% of colleagues who make decisions about ratings identify as being from an ethnic minority background (due to small numbers, the underlying figures are not available). Thirty-two per cent (65/204) of GP specialist advisors are from an ethnic minority background and 30% (61/204) from a non-ethnic minority background. The other 38% of GP specialist advisors did not state their ethnicity.
The diversity of inspection teams is perceived to have an impact on inspection outcomes. In the GP practice survey, practices were asked whether they agreed that they would have achieved the same inspection outcome with a different inspection team. Forty-one per cent (165/402) of ethnic minority-led practices indicated that they would, and 25% (102/402) indicated they would not (note: for this question, eight ethnic minority-led practices answered ‘not applicable’, so we removed these responses from the denominator).
For non-ethnic minority-led practices, 50% (168/339) indicated they would have achieved the same inspection outcome with a different inspection team, and 20% (67/339) indicated they would not (note: 10 non-ethnic minority-led answered ‘not applicable’ and were removed from the denominator). Results were similar among practices that did or did not serve socio-economically deprived patient populations.
Practices were asked whether inspection teams’ awareness of equality, diversity and unconscious bias affected their practice’s most recent inspection or rating. There were primarily neutral responses to this question, with practices indicating that they neither agreed nor disagreed with this statement. This may be because it is difficult for GPs to be able to give a definitive answer about the awareness of inspectors, unless there was evidence of a specific action of an inspector (82 out of 410 ethnic minority-led practices and 101 out of 349 non-ethnic minority-led practices did not provide an answer). However, 31% (101/328) of ethnic minority-led practices indicated that inspection teams’ awareness of equality and diversity had negatively affected their inspection/rating. In contrast, only 2% (5/248) of non-ethnic minority-led practices thought this was the case.
Recognition of local needs and innovation:
Ethnic minority GPs in the online research community highlighted that they would value a greater understanding by CQC inspection teams of local areas and populations and the day-to-day realities of general practice. They also felt that CQC inspection teams could be more supportive, with improved, more open communication between CQC and practices.
Concerns were also raised in the online community about a lack of recognition of innovative practices that work to meet the needs of patients in areas of deprivation.

“Inspection team should be more diverse and reflect the make-up of GPs working in the NHS. CQC should understand practices are very different and take this into consideration, particularly looking at the demographics of the patients being looked after and appreciating the challenges faced by GPs, and look to show excellence and positive care working in such adverse conditions rather than always looking for negatives.”
(Male, Indian, Midlands)
Inspection processes:
To find out how our systems and processes may affect ethnic minority-led practices, we reviewed our inspection methodology and how it is applied. We asked questions to explore whether there was a perception that ethnic minority-led practices are treated differently to non-ethnic minority-led practices.
Evidence used to inform inspections:
CQC uses the most up-to-date, high-quality information to review practices’ performance. We routinely monitor and follow up on key national data indicators during inspections and communications with the practice. The data we currently hold looks at:
- uptake for routine screening and immunisations to prevent serious illness
- access and patient experience as captured in the NHS GP Patient survey
- levels of prescribing.
In our GP practice survey, 31% (117/381) of ethnic minority-led practices felt negatively affected by indicators that were used. For non-ethnic minority-led practices, this was 12% (37/313). Thirty-three per cent (118/357) of providers whose practice served socio-economically deprived patient populations felt negatively affected by the indicators used by CQC, compared with just 10% (35/336) of practices not serving socio-economically deprived patient populations. (Note: 65 ethnic minority-led and non-ethnic minority-led respondents answered ‘don’t know’ to this question and have been excluded from the denominators.)
While participants in the inspection team focus groups and interviews felt there was no difference between regulating ethnic minority-led and non-ethnic minority-led practices, some felt that the way evidence (in particular data) is considered during the inspection process could be perceived to disadvantage some ethnic minority-led practices that might be more likely to work in challenging circumstances.
Patient choice and autonomy could lead to lower levels of engagement with GPs in respect of the uptake of patient screening and immunisation. For instance, the participants in the focus groups and interviews noted how some patients may be unwilling to participate in immunisations, while other patients were thought to carry out aspects of their health care (including immunisations and screenings) outside the UK. As such, GP datasets were affected if they served populations behaving that way, leading to discrepancies in practice evidence and potentially affecting inspection outcomes.
Participants in the inspection team focus groups and interviews identified two prominent measures used in the monitoring and assessment of practices as being influenced by sociocultural factors: cytology (cervical smears) and childhood immunisations. These measures were flagged by most of the participants as having a potentially negative impact on monitoring and inspection outcomes for GP practices that serve ethnically diverse communities. Participants suggested that practices needed to show evidence of their efforts to increase uptake.

“If they can demonstrate to us that they are doing all that they can to bring patients in [for childhood immunisations and cervical screening], then we will take that into consideration.”
(CQC inspector).

“I’m of the opinion that if you know [that] a practice is aware of it, and doing everything within their power to demonstrate that they're trying to make it better, then we've got to take that into consideration.”
(CQC inspection manager).
While national targets rather than CCG averages are used in relation to cytology (cervical smears) and childhood immunisations, participants in the focus groups and interviews of inspection teams highlighted how using CCG averages in relation to other indicators could be of concern when practices were located in pockets of deprivation.

“In my CCG as well, [name of CCG], we've got areas of like say [name of area 1] which is high deprivation, higher ethnicity and stuff like that. Yet, a mile away we've got like [name of area 2] where celebrities live. We've got these multi-million pound houses and when we look at it as a whole and as a CCG, they just can't compare because they’re looked at as a CCG for [CCG name] nationally. It’s almost like I know we can't but, looking into it differently and just how to use data and add in that context to explain why data may be poor […].”
(CQC inspector)
However, we also heard from these participants that CQC should not compromise on standards, as people in deprived and/or more diverse areas deserve equally safe, good quality care. One inspection manager pointed out that, despite the challenging circumstances some practices operate in, targets such as cervical cytology should not be put aside, as doing so could result in poorer health outcomes for people in deprived areas.
We heard from CQC colleagues and specialist advisors that the way CQC considers patient feedback may inadvertently disadvantage ethnic minority-led GP providers. Feedback mechanisms, including CQC online feedback forms and reviews from NHS Reviews are in English and may therefore exclude some parts of the population from participating. This is significant for ethnic minority-led practices as they appear to serve populations where English proficiency may be lower. This may limit response rates and systematically exclude some parts of practice populations. We also heard that on-site feedback gathering may also be restricted due to language and cultural barriers.

“If you serve ethnic minority patients, I'm certain, I haven’t got evidence, but I'm certain that they are less likely to send in compliments. You're less likely to get feedback in the Friends and Family Tests, even less likely to get any of that.”
(CQC specialist advisor)
CQC's terminology:
In the focus groups with inspections teams, language was identified as a factor affecting the ability of ethnic minority-led GP practices to meet CQC data requests and regulation requirements. Specifically, this related to the terminology and jargon CQC uses in its guidance and processes.
Participants said that CQC has a specific way of communicating, which very often did not align with that of different services and practices.

“Often the language used by CQC in its written published guidance and during inspections can be difficult to understand especially for [ethnic minority-led] practices, and practices where the interviewee holds English as a second language. During inspections, I find myself having to ‘translate’ the key questions during an interview so the interviewee has the best chance in understanding the nuance of the question and can therefore answer it to the best of their ability. I can imagine this does not happen consistently and therefore are we affording the best chance to those being inspected.”.
(CQC specialist advisor)
Our GP practice survey asked practices how the clarity or availability of CQC’s guidance affected the practices’ rating and/or inspection. Eighteen per cent (61/341) of ethnic minority-led practices said that this had a negative impact, compared with 3% (9/277) of non-ethnic minority-led practices. Nevertheless, 23% (80/341) of ethnic minority practices said that it had a positive effect and 59% (200/341) said that it neither positively nor negatively affected the rating and/or inspection. (Note: 141 ethnic minority-led and non-ethnic minority-led practices answered ‘don’t know’ to this survey question and were excluded from the denominators.) This would suggest that ethnic minority-led practices are more likely to find the guidance difficult to use than non-ethnic minority-led practices, although guidance remains an issue for a small number of practices.
In the focus groups with inspection teams, it was noted that CQC guidance documents are not available in other languages. This may limit GPs and other practice staff whose English proficiency restricts them from fully understanding regulatory expectations and associated data collection requirements.
Quality assurance processes:
Before publishing an inspection report, we carry out quality checks to ensure our judgements are consistent and fair. All inspection reports go through a robust quality assurance process before they are published. There are a number of scenarios where a draft report would go to a quality assurance panel, including when a draft report indicates that the practice will be rated as inadequate.
Participants in our senior leaders’ workshop explained that when inspection reports go to quality assurance panel, the review is rigorous to ensure consistency and quality of judgements. They explained that significant time is dedicated to review outliers in data, including those that are rated as inadequate as well as those that are rated as outstanding. They believe that the conversations around what would constitute poor practice are consistent.
In the GP practice survey, participants were asked about the impact of CQC’s quality assurance procedures. Overall, 48% (369/771) of providers were neither positively nor negatively affected by CQC’s quality assurance procedures, and 28% (214/771) of providers ‘didn’t know’. While the numbers of those who said that they were negatively affected by the quality assurance procedures was relatively small, this was over three times higher when comparing providers from ethnic minority-led practices with non-ethnic minority-led practices (23% (73/316) compared with 7% (17/233) when considering practices that provided a response, that is they did not respond that they ‘didn’t know’).
In the review of a sample of 30 GP practices whose inspection reports had been through CQC quality assurance processes, we found no reference to consideration of issues that were likely to disproportionately affect ethnic minority-led providers – for example, being led by a single-handed GP or having a patient population with high deprivation or significant ethnic diversity. In one case, a rating for a key question was lowered partially on the basis of low uptake of cancer screenings. In the factual accuracy part of our methodology review, several providers identified this as being more likely to happen among populations with high ethnic diversity who can be less willing to participate in intimate screening processes, and therefore challenged (unsuccessfully in all cases) through the factual accuracy process as a result.
Of the 10 reports in the sample that went to the quality assurance national panel, one had its proposed overall rating lowered from requires improvement to inadequate. This provider self-identified as non-ethnic minority-led. In five other reports, individual key question ratings were lowered, but with no change to the overall rating. Four of these reports were for providers that self-identified as ethnic minority-led or had a majority of partners who qualified outside the UK.
For two reports, ratings for individual key questions were upgraded, although following aggregation principles, this made no change to the overall rating. One of these reports was for a provider that self-identified as ethnic minority-led or had a majority of partners who qualified outside the UK; the other was not.
It is worth noting that contextual factors were applicable in these panel reviews, as nine out of 10 reports that went before the national panel were for providers with deprivation scores of 5 or below, with six of these having scores of 1 or 2, indicating that they are based in areas among the most deprived in the UK.
In the inspector survey, 69% (37/54) of respondents did not agree that ethnic minority-led GP practices were treated less favourably by quality assurance panels because of unconscious bias and discrimination; 9% (5/54) agreed. Also, 44% (24/54) disagreed that ethnic minority-led GP practices were treated less favourably by quality assurance panels because of the types of practices or environments they work in (for example, areas of deprivation or being single handed GPs). However, 37% (20/54) of respondents agreed with this statement. This was to some extent reflected in examples in discussions with inspection teams in the focus groups. Some participants recounted how evidence presented to mitigate some performance indicators that fell below the expected standard, or some evidence for outstanding practice, was not considered in quality assurance panels. In those instances, they felt that ethnic minority-led practices, which face greater challenges and therefore may not be able to produce the type of evidence quality assurance panels expect, may be at a disadvantage.
Decisions about enforcement:
Management review meetings take place to support inspectors’ decision-making around risks identified during monitoring activity or on inspection.
We considered 30 management review records as part of the methodology review. Ten were instigated because of risks identified following inspection, seven owing to concerns with leadership within the practice, seven as a result of a routine risk review and six in response to other information of concern such as receipt of a safeguarding notification or whistleblowing, or risks identified as part of routine reviews during the COVID-19 pandemic.
All seven of the practices experiencing issues with leadership were among those that had self-identified as ethnic minority-led or had a majority of partners who qualified outside the UK. Issues with leadership included retirement or illness of a GP partner, or break-up of the business partnership. Of these seven practices, one was made subject to an urgent suspension, one to urgent conditions, two to warning notices, two to further inspection and one to ongoing monitoring.
Overall, in the sample of 30, practices that were ethnic minority-led or those where a majority qualified outside the UK had a higher number of enforcement actions applied. Of the 14 decisions made about further regulatory action in management review meetings, nine related to providers who self-identified as ethnic minority-led or had a majority of partners who qualified outside the UK. The regulatory action taken against these nine practices included five warning notices, one imposition of urgent conditions, one suspension, one imposition of special measures and one requirement notice.
Factual accuracy challenge process:
In the survey of inspectors, a small number (7% (4/54)) agreed that factual accuracy challenges raised by ethnic minority-led practices were less likely to result in changes to the inspection report; 56% (30/54) disagreed.
In the review of factual accuracy processes, 16 practices identified as being ethnic minority-led or were led by a majority of GPs whose country of qualification was outside the UK. Of these factual accuracy submissions, seven related to factual errors in the report, three to incomplete evidence referred to in the report, three to typographical errors, two to confirm that no changes were required, and one that suggested ratings changes.
There was some inconsistency in our responses to factual accuracy challenges. Three different forms had been used during our review period, and we found that factual accuracy forms were not always clear in describing why challenges had been accepted or not. This may mean that providers were less able to decide whether to use other processes to further challenge the report.
Challenging inspection outcomes:
There are processes to enable CQC to hear and respond to concerns during and after the inspection process. Practices can raise a complaint at any point during the inspection process, although not all complaints will be fully dealt with at the time, depending on what other action is currently being taken. Practices may request a review of the ratings following publication of an inspection report.
In our GP practice survey, 29% (98/335) of ethnic minority-led providers felt negatively affected by the ability to challenge ratings through feedback mechanisms, compared with 11% of non-ethnic minority-led providers (30/261). (Note: 163 ethnic minority-led and non-ethnic minority-led practices answered ‘don’t know’ and have been excluded from the denominators.)
In the online research community, some GPs from an ethnic minority background felt there was a possible risk of victimisation, poorer ratings or re-inspection if they chose to raise complaints. They highlighted the importance of clear, transparent and accessible processes to challenge inspection outcomes.

“I was told that to query the inspection may trigger another inspection and I definitely did not want to go through that again.”
(Male, Indian, Midlands)

“Need to be able to challenge CQC decisions if ethnic minority-led GP practice felt the outcome of the rating was unfair, not objective, not replicable and not transparent.”
(Male, Black, East of England)
Ethnic minority GPs in the online community felt that there should be a robust and independent process for appeals, as well as mechanisms for redress in case a complaint is sustained. While there are systems in place that seek to ensure objectivity in our review processes, it may be the case that these are not clearly understood by providers. This suggests that CQC needs to more clearly communicate these appeals processes to instil trust in the inspection process.

“Appeals against CQC inspection outcome should be heard independently, heard quicker and be easier to access, before an inspection report is published. I think the number of successful appeals is very, very low.”
(Male, Pakistani, North West England)
Complaints:
Complaints can be about the conduct of CQC employees or a failure to apply due process. They cannot be about evidence that CQC relies on following an inspection or any resulting enforcement action, as there are other available mechanisms to raise challenges of this nature.
Between April 2016 and March 2021, there were 167 complaints made by NHS GPs to CQC. Thirteen of these related to bias, discrimination, racism or protected characteristics. Specifically, complainants raised concerns about the conduct of, or questioning by, inspection teams and the application of our processes. Of these 13 complaints, 12 were progressed and one was withdrawn. Of those progressed, two were upheld, six were partially upheld and four were not upheld.
Recap
Our research identified several factors that may be associated with differences in ratings, outcomes and experiences.
Factors internal to ethnic minority-led practices:
- Single-handed/individually led practices – these are more commonly associated with being ethnic minority led. The time-consuming nature of inspections can be harder for smaller practices.
- Practice management/leadership – practices may be more likely to be run by GPs less familiar with CQC regulation or with poorer IT skills, and leaders less able to provide evidence at inspections. This may reflect a need for CQC to be more considerate of these differences to better support practices.
Factors external to ethnic minority-led practices:
- Levels of deprivation – socio-economic deprivation was identified as a challenging factor by both GPs and CQC inspectors, as it can affect GP practices’ ability to achieve national targets considered as part of CQC inspections. Some CQC inspectors and specialist advisors felt there was limited recognition within CQC’s approach of the surrounding context of practices, and practices are penalised for not achieving similar outcomes to those with very different contexts and patient communities. Deprivation can also affect recruitment and funding.
- Population health – patients with poorer health typically need more care from their GP practices, increasing the practice’s workload.
- Support from external bodies – ethnic minority GPs felt that their ethnicity had an impact on the level of leadership support they received from other bodies
- Interaction with patients – some ethnic minority GPs reported experiencing racism from patients, especially when patient expectations could not be met. They also felt patients were more likely to raise a complaint about an ethnic minority GP than a White British GP, although it was reported that racist incidents had decreased in recent years.
CQC factors:
- Objectivity and consistency – CQC’s need for objectivity and consistency was seen to potentially have a negative impact on ethnic minority-led practices, as it may lead to unfair outcomes where the methodology is not sufficiently tailored to reflect providers’ circumstances. However, CQC colleagues emphasised that their key priority was ensuring that care was safe and accessible, regardless of the challenging circumstances that practices might face.
- Recognition of innovative practice – concerns were raised by GPs that CQC did not take account of innovative practices to respond to local needs. Ethnic minority GPs felt inspection teams needed greater cultural competence, including understanding local areas and populations. There was appetite for a more supportive and open relationship between CQC and practices. Diversity of the inspection team was also raised, with concerns that inspectors were largely White, so they may not understand the experiences of ethnic minority GPs.
- Inspection processes – evidence used in inspections was perceived to disadvantage both ethnic minority-led practices and practices serving socio-economically deprived patient populations. Patient behaviours, such as their hesitancy to receive vaccinations, affected practices’ performance, particularly when compared with national targets. Similarly, website reviews and online feedback forms could disadvantage practices serving communities with lower levels of English proficiency.
CQC’s terminology might impede ethnic minority-led GP practices from meeting data requests and regulation requirements.
We identified some inconsistencies in our responses to factual accuracy challenges, and we were not always clear in our decision making. While we didn’t identify any specific inconsistencies for ethnic minority-led practices, this could mean that all providers were less able to decide whether to use other processes to further challenge the report.
Ethnic minority-led practices were more likely to feel negatively affected by the ability to challenge ratings through feedback mechanisms, with some ethnic minority GPs identifying a possible risk of victimisation, poorer ratings or re-inspection if they choose to raise complaints. They highlighted the importance of clear, transparent and accessible processes to challenge inspection outcomes and felt there should be a robust and independent process for appeals, as well as mechanisms for redress in cases where a complaint is upheld or partially upheld.
Research question 3: What improvement could CQC consider to help promote equity in ratings, outcomes and experiences?
In our Equality Objectives for 2021-25, we pledge to support the reduction of inequalities not only for people who use services but also for those that provide them. As a result, we want to use this work as an opportunity to understand how we as the regulator can improve, move forward and plan for the future.
Action to ensure equity of treatment for practices and to benefit patients
Consideration of practice context in CQC’s methodology:
GPs from ethnic minority-led practices who participated in our online research community told us that they want CQC’s methodology to consider the specific challenges that their practices face, and tailor the inspection process accordingly. This could involve taking into account the practice population and ensuring inspection reports reflect that lower ratings may be because of additional external pressures rather than poor clinical work or a lack of concern by the practice for the wellbeing of their patients.
A similar theme was identified in our focus groups with CQC inspectors, inspection managers and specialist advisors. Colleagues expressed that it could be beneficial to understand the practice context for ethnic minority-led practices. These suggestions were less about supporting GPs to meet the regulations and more about the ability of inspectors to consider the contextual factors surrounding a GP practice within the structure of the regulatory framework and inspection methodology. Although not necessarily an issue only faced by ethnic minority GPs, participants had a general sense that ethnic minority GPs were more likely to work in areas of greater ethnic diversity, deprivation and health inequalities. It was suggested that the contextualisation of these factors when interpreting data, using multiple sources of evidence to look at care quality and safety, might move to a more holistic assessment of quality. As one inspection manager noted, some practices have to go the “extra mile” and this should be recognised by CQC.
A more supportive approach:
In our GP practice survey, 72% (557/771) of respondents told us they engaged with inspectors at some point during the inspection process. Fifty per cent (367/738) of respondents felt that discussions with the CQC inspector helped to prepare for the most recent inspection (note: 33 respondents answered ‘not applicable’ for this question and were excluded from the denominator). However, 70% (38/54) of the inspectors we surveyed felt that the inspection outcome would not have changed if the practice had engaged more with the inspection team, although 7% (4/54) indicated that the outcome would have changed. Twenty-two per cent of inspectors (12/54) did not have a view on whether more engagement with inspection teams would have changed the inspection outcome.
Ethnic minority GPs in our online research community told us they hope to see a more interactive and supportive approach from inspections in the future. They told us they wanted better communication with inspectors to address their concerns. For instance, GPs said that they would like more clarity around expectations, and more transparency about CQC processes and decisions about ratings.
CQC colleagues expressed similar views to those of GPs in the online community. For example, one inspection manager explained that they had seen the advantage of more frequent, less formal interactions with practices during the pandemic. In the focus groups and interviews with inspection teams, participants observed that the engagement the inspectors had with the practice was influential in both creating rapport between the inspectors and GPs. A good rapport with GPs opens the way for a better working relationship and discourse, where GPs can feel more comfortable asking questions around meaning and what’s expected of them.

“But again, it depends on the inspector and the approach they take. For example, in some areas I've seen that the inspector has a good collaboration with people and encourages them to do things, is actually is kind of trying to get them through things constructively.”
(CQC specialist advisor).
Access and engagement:
Encouraging access and engagement with CQC guidance and materials was seen as another area for improvement. While 76% (589/771) of GP practice survey respondents stated that they accessed or engaged with CQC guidance and materials at some point during the inspection process, there were differences in how inspectors felt this activity would have affected an inspection outcome. Forty-three per cent (23/54) of inspectors surveyed agreed that the inspection outcome for ethnic minority-led practices was likely to have been better if the practice had accessed CQC’s guidance on the website. However, for non-ethnic minority-led practices, an equal number of inspectors surveyed (12) agreed and disagreed (38% and 38%).
Inspectors, inspection managers and specialist advisors we spoke to felt that CQC could play a bigger role in supporting GPs to understand the regulatory framework and help them understand the requirements and expectations. This included providing training about CQC’s five key questions (are practices safe, effective, caring, responsive and well-led?) and by simplifying the language used in inspection reports. Other ideas involved pointing GPs to examples of good practice on CQC’s website, so they understand what a rating of good entails, inspectors sharing good practice that they have seen in other practices, and making newsletters clearer, simpler and more accessible.
The importance of positive engagement between CQC and ethnic minority-led GP practices was also a theme identified by both parties. GPs in our online research community felt that a friendlier, less combative approach would allow GPs to have more discussions about their concerns without the fear of repercussions. Similarly, CQC colleagues told us how having a supportive rather than a perceived punitive attitude towards GP practices would help practices to take on board suggestions for improvement. For example, delivering an inspection report in person, having informal conversations, talking to GPs about their experiences, better portfolio management, additional engagement after concerns have been flagged and proactive relationship building were proposed as ways to offer better support.
A greater focus on partnership working was also suggested by both CQC colleagues and ethnic minority GPs. In our survey of GP practices, 43% (314/732) of respondents strongly agreed or agreed that concerns raised by the practice were given due consideration during the inspection process, and 25% (186/732) disagreed or strongly disagreed with this statement (note: 39 respondents answered ‘not applicable’ for this question and were excluded from the denominator). When looking at practices that are ethnic minority-led, 17% (68/396) strongly disagreed with this statement. In comparison, only 6% (19/326) of non-ethnic minority-led strongly disagreed. As such, ethnic-minority GPs in our online community suggested that CQC could do more to signpost support available to deal with specific issues. Similarly, CQC colleagues commented that inspectors could do more to encourage improvement.
Factors outside of CQC’s role where we could use our influence
Support from system partners:
GPs from our online community also commented on the support they receive from the wider system. GPs often work with other organisations and bodies to improve the quality of care they provide, and these interactions may influence their inspection ratings and outcomes. While the focus of this report is on CQC’s regulatory approach, we are able to use our regulatory influence to shine a light on and call for action on wider issues.
Ethnic minority GPs in our online community stated that primary care networks (PCNs) are often well placed to provide support such as advice on CQC inspections and how to prepare for them. They were also able to provide a forum to share learning and act as facilitator to improve system collaboration between GPs, clinical commissioning groups (CCGs) and local medical committees (LMCs). CCGs and LMCs were also referred to as sources of system support, although there was a feeling that they could do more to support practices through CQC inspections.

“The best placed local organisations I feel are the CCG, more recently the PCNs and LMC. The CCG and LMC in particular could be more hands on, provide tailored support and even better [if] they have designated advice teams.”
(Male, Indian, North West)

“CCGs and PCNs do work to support practices. They do seem to help us. However, they could do more for each practice to give them good CQC guidance on how to pass.”
(Male, Black, North West)
Participants in the focus groups with inspectors, inspection managers and specialist advisors told us they had seen how CCG support initiatives had made a positive impact. One inspection manager explained how the support provided by a CCG had enabled significant improvement across all practices in special measures in that area. In this case, the approach by the CCG had led to all local practices coming out of special measures.
It was felt that there was a lack of clearly set out roles and responsibilities around supporting GPs in inspection outcomes and ratings. CQC inspection staff generally felt that a support role sat within the remit of CCGs rather than with CQC. Some inspectors had experiences where the CCGs had not supported practices because they believed CQC would do so. This would suggest that at least some CCGs believed these responsibilities sit with CQC. To address this, there were suggestions that working relationships between CQC and CCGs could make a difference, for example by inspectors having conversations with CCGs about how practices could be supported and to set out roles and responsibilities around this. However, there was also a view that this should not be the role of individual inspectors to have those conversations.

“I think we need to engage better at a more senior level with these partner agencies. Often it can be left to the inspector when we have found problems. When you're working in a reactive way, you're very focused on that specific practice in that specific risk. You're not talking across the geographical area and looking at why that practice in that inner city is struggling. We don't have those strategic conversations that need to happen at a higher level on a regular basis.”
(CQC inspector)
Some GPs from our GP practice survey also reported that they sought support (over the last five years) from other system partners such as NHS England and NHS Improvement (NHSEI), the General Medical Council (GMC), the Royal College of General Practitioners (RCGP) and the British Medical Association (BMA). Interestingly, 78% (598/771) of respondents stated that they did not seek any support from NHSEI and 90% (692/771) of practices did not seek support from the GMC. These findings were similar between ethnicities and levels of deprivations present in practices. Seventy-two per cent (556/771) of providers did not seek support from the BMA. Of ethnic minority-led providers who did seek support from the BMA, 43% (43/101) got support and felt it was good. In contrast, 67% (74/111) of non-ethnic minority-led providers received good support from the BMA. The findings were similar when comparing practices serving socio-economically deprived areas with those serving non-deprived areas.
In our focus groups with inspectors, inspection managers and specialist advisors, we heard that there may be a need for additional support for GPs who trained abroad and therefore may not be familiar with UK systems and processes.

“For providers that maybe have been trained in a system that isn't in the UK or somewhere that has a similar system to us, or even, if you like, grown up in the system like this, I think that they start off on an unfair footing really. Because if you have developed in a different system to ours and you [don’t] know the systems that we have and the things that we look at or what primary care looks at. For a doctor trained in this country it takes a long time for them to get to the point where they're able to successfully manage and navigate the health care landscape. If you've come from a system that's different, that must be incredibly difficult for doctors coming in to do that. It would be really good if […] someone could have some support in place to share that information with them.”
(CQC inspector)
Recap
Our research revealed suggestions for improvement for both CQC and the wider sector.
Both GPs and inspection teams felt there could be more in CQC’s methodology to reflect the specific context in which GP practices operate. Practices wanted to see a more supportive approach from CQC. In our surveys, half of the GPs that responded reported that discussions with CQC inspectors helped them prepare for inspection, but inspectors felt that engagement does not affect inspection outcomes. Practices wanted to see better communication with inspectors and greater transparency about expectations, processes and decision-making.
It was also felt that CQC should encourage better engagement with guidance and materials aimed at practices, and help practices understand requirements and expectations. Simplified language in communications and reports, training for providers on the inspection methodology, sharing examples of good practice on the website, and better signposting to available support were all suggested. Practices felt that moving away from what was perceived to be a punitive approach to regulation would support providers and patients alike, as providers could discuss concerns without fear of repercussions, helping them to work with CQC to improve.
A consistent theme from ethnic minority GPs was about the support they receive from the wider system. CQC inspection teams generally felt that the role of supporting providers sat with CCGs as opposed to CQC. However, some inspectors had experience where CCGs had not acted to support practices as they thought it was CQC’s role, suggesting that there is a lack of clarity of roles and responsibilities when it comes to supporting GP providers. It was suggested that CQC and CCGs needed to improve their working relationship and increase dialogue about the support practices need. It was felt that improving this relationship should not be the responsibility of individual inspectors.
Other partners in the system, such as the BMA, the GMC and NHSEI, were also highlighted as having a supportive role. As with CCGs, where ethnic minority-led practices did seek out support from these partners, they were less likely to report this was good. However, CQC inspection teams suggested that there might be a need to support GPs who have trained abroad and therefore may not be as familiar with UK systems and processes.
Conclusion: learning from what we found
This programme of work was designed to look at our own systems and processes and how these affect inspection outcomes for ethnic minority-led GP practices. As an organisation, there is still work for us to do to ensure that we achieve our strategic and equality objectives and deliver our core purpose to ensure that we encourage practices that need support to improve.
This work has identified an inter-relationship between factors that can lead to poorer regulatory outcomes. Internal or practice factors often have a disproportionate impact on practices where many ethnic minority GPs work. Ethnic minority-led GP practices are often operating single-handedly, which results in challenges in support, resourcing and capacity. These additional burdens affect the ability of a practice to show evidence that it is meeting regulatory requirements.
Importantly, there are also wider, contextual factors that affect ethnic minority-led GP practices – in particular the efforts required to respond to the health inequalities of patients in areas of deprivation. Practices in areas of deprivation struggle with lower funding and systems of support. This work has demonstrated the need for better system-wide engagement in addressing these factors and we hope to further this conversation through the findings from this report.
Our primary purpose is to ensure that people receive safe, high-quality health and care services. However, some aspects of CQC’s inspection and monitoring methodology may inadvertently disadvantage practices due to the factors above, leading to inequities. We need to capture and consider the challenging circumstances that ethnic minority-led practices are often working in, while not lowering standards of care. Although we will continue to ensure that all patients can expect to receive the right care at the right time, we must ensure we are doing everything we can to encourage improvement, rather than risking perpetuating the cycle of inequality.
What we are already doing
We are already taking action to improve in a number of areas related to the findings from this review, which we will continue to progress.
- We are continuing our work through the Regulators’ Pioneers Fund, which will support us to identify innovation in areas of deprivation and share good practice as part of our routine regulatory processes, assessments and engagement. This will enable us to recognise more responsive care and good leadership where a GP practice is operating in more challenging circumstances.
- As part of our ongoing work to embed our new strategy, we are developing how we can work more closely with providers, so we have a better understanding of providers and the needs of their populations, and to encourage more open and transparent communication as we move to assessing providers on an ongoing basis.
- Our Diversity and Inclusion strategy aims to increase the number of ethnic minority colleagues at all grades, but especially at senior leadership levels.
What we will do next
We will take the following actions to respond to the findings from this review.
1. The Health and Care Bill places a new duty on CQC to review and assess integrated care systems. As we develop our approach to do this, we will consider how we can focus on reducing inequalities for people who use services. In doing this, we want to address where local systems need to provide more support to ensure that primary care meets the needs of everyone in their population.
2. We will carry out further work to understand the systemic factors that have the potential to adversely affect the ability of some ethnic minority-led GP providers to deliver high-quality, safe patient care and better health outcomes for their populations.
3. We will continue to work with our system partners in the sub-group of the Primary Care Quality Board to identify and progress shared priorities in ensuring equality for ethnic minority-led GP practices and the populations they serve. The priorities that we want to explore from this work include:
- Reviewing and improving ways to capture feedback from diverse ethnic groups about the care they receive
- Reviewing what can be done within the wider system to ensure that single-handed practices are not unduly disadvantaged by the circumstances in which they work.
- Reviewing whether the current arrangements for supporting GP practices are effective for those in areas of deprivation that are experiencing disproportionate pressures, such as professional isolation and lack of funding. As part of our strategic ambition to accelerate improvement, we will consider how we encourage and work with all GP practices to access support to improve.
4. While continuing to expect good quality of care for everyone, we will review and refine how we assess GP practices and reach our judgements about quality and ratings. We will strengthen how we consider the context in which a GP practice works. This can include:
- Reviewing how we use evidence about the efforts that GP practices are making to respond to the health inequalities of their practice populations as well as the outcomes of those efforts.
- Ensuring that we reflect factors that could disproportionately (although not exclusively) disadvantage ethnic minority-led GP practices in our decision-making processes, without compromising on expected standards of care for people. These factors include operating single-handedly and professional isolation. This will enable us to recognise more responsive care and good leadership where a GP practice is operating in more challenging circumstances.
- Reviewing our quality control and assurance processes to consider whether we can do more to remove the risk of any potential bias.
5. We will clearly explain our inspection and assessment processes and expectations of all providers so they are easy to understand. To do this:
- Inspection teams will continue to build ongoing relationships with GP practices to help them understand our regulatory approach and requirements.
- We will support all GP practices to understand how to give feedback, challenge our reports and ratings, and raise complaints. This will include reviewing our guidance (including factual accuracy and ratings review processes) to ensure it is clear and accessible to all providers and to inspection teams that support GP practices.
6. We will support our inspection teams to understand the contextual factors that affect ethnic minority-led GP practices. To do this, we will provide more targeted and mandatory learning for inspection teams, so they understand the contextual factors that are important when assessing GP practices.
7. We will develop with others our approach to collecting ethnicity data. This will enable us to continually analyse regulatory outcomes such as ratings and enforcement by whether practices are ethnic minority-led and will help us determine what further actions may be needed.
Appendices
Appendix A: Statistical model for ratings
We set out to perform statistical modelling to understand whether there is an association between the ethnicity of doctors working in a practice and CQC ratings after taking into account:
- characteristics of GPs working in the practice (for example, ethnicity, place of qualification, time since qualifying)
- characteristics of GP practice patient lists (for example, age and health profile of patients)
- characteristics of the local area (for example, deprivation, urban or rural location)
- characteristics of the practice (for example, contract type, number of patients per GP, whether a practice is single-handed)
- Quality and Outcomes Framework (QOF) indicators used by CQC when monitoring and rating practices
- results of the NHS GP Patient Survey
- other data for GP practices that CQC holds (for example, number of complaints, number of whistleblowing events).
We asked the General Medical Council (GMC) to provide data to enable us to carry out the statistical modelling and received data on:
- the number of GPs working in each practice that are from an ethnic minority background, the number of GPs that are not from an ethnic minority background, and the number of GPs that have not declared their ethnicity
- the proportion of doctors in each practice that have qualified in the UK, the European Economic Area (EEA) or elsewhere
- the average length of time since doctors in each practice had received their first licence
- the proportion of doctors in each practice that are female and male
- the average age of the doctors in each practice.
The remaining variables for this analysis were either already held by CQC or were prepared from publicly available data sources.
However, the data available were not sufficiently complete to perform effective statistical modelling that would ensure that any conclusions were robust and based on good evidence. This was caused by the following limitations:
- Full ethnicity data was not available for most practices. The main reason for this is that not all GPs working at a practice had reported their ethnicity to the GMC, either because they opted not to disclose the information or because the information was not being collected when they registered. There were also secondary reasons relating to matching the data provided by the GMC to internal data for CQC-registered locations. This left a sample of about 20% of practices with full ethnicity data linked to a recent (comprehensive) inspection, amounting to 1,324 practices (note that this is 20% of all GP practices, rather than GP providers as per our survey – some providers run more than one practice).
- In addition to the small sample size, the number of GP practices that were rated overall as requires improvement or inadequate was low: 100 practices out of 1,324 practices with full ethnicity data. Although this proportion is representative of all inspections, the fact that it is low means that it is unlikely a model will be able to detect a relationship between the ethnicity of doctors working in a practice (or other factors) and ratings, even if such a relationship exists. (To illustrate this: a model that simply says that all practices have been rated as either outstanding or good is in itself a pretty good model since most practices have indeed been rated as either outstanding or good. However, such a model is clearly not useful in practice.)
- Key variables that would need to be included in the model were missing, for example the health profile of the patient population or results of patient satisfaction surveys. These variables are collated using data from the NHS GP Patient Survey, the questionnaire for which was changed in 2018. This included changes in the wording of the questions as well as who is eligible to participate in the survey. Consequently, we do not have consistent historical data for variables collated from the survey. Without these, we would have had low confidence in the results of the model. For example, if we found a relationship between the ethnicity of doctors and our ratings, we would not be able to rule out that this was because practices with a high proportion of ethnic minority doctors serve populations with a higher prevalence of long-term health conditions.
Lastly, it is important to highlight that even if we had estimated a statistical model, we would not have been able to establish whether there was a causal relationship between GP ethnicity and CQC ratings. An example to demonstrate this is that practices with lower ratings may have issues recruiting because doctors prefer to work in practices with higher ratings. If there is bias in the recruitment process (that is, if practices are less likely to recruit ethnic minority doctors because of bias), then GP practices with lower ratings are more likely to have a higher proportion of ethnic minority GPs. However, the bias in this case is at the recruitment process rather than the inspection process.
Appendix B: Terms of reference for the sub-group of the Primary Care Quality Board
Sub-group of the Primary Care Quality Board on inequalities faced by ethnic minority-led providers in primary care.
1. Background and context
- To address concerns in the primary care sector that ethnic minority-led GP practices are more likely to receive lower ratings from CQC and to explore the challenges that ethnic minority-led practices may disproportionately face in meeting their regulatory, legal or commissioning requirements.
- The sub-group brings together bodies that have a role in improving the quality of primary care and/or supporting primary care providers and healthcare professionals in England. These bodies include organisations that represent ethnic minority providers and healthcare professionals.
2. Purpose
- The sub-group will formally report and be accountable to the Primary Care Quality Board. It will provide a quarterly report to the PCQB.
- The sub-group will work together to address inequality issues faced by practices led by ethnic minority groups.
- The purpose of this sub-group will be to:
- develop a shared understanding of inequality issues faced by practices led by ethnic minority groups
- provide a forum for members to discuss lived experiences and discuss both internal and external facing projects
- share learning and improvement across the whole of primary care services
- minimise the risk of duplication and missed opportunities for learning from others
- identify opportunities for partnership working and coordinate joint activity while maintaining clear lines of organisational accountability and individual organisational action
- develop recommendations for system-wide improvements to address inequality issues faced by primary care services.
- The subgroup will monitor progress on the agreed programme of work to reduce inequalities faced by ethnic minority-led practices.
| Deliverable | Lead organisation(s) | Timescales |
|---|---|---|
|
Definition of ethnic minority-led practices for system-wide use Recommendations for how to apply the definition and data collection requirements |
CQC CQC/GMC |
2021/22 Q2 2021/22 Q2 |
| Project looking at inequalities faced by ethnic minority-led GP providers in CQC ratings | CQC | December 2021 |
| Work to collect ethnicity data through professional standards | NHSE/I Professional Standards | |
|
Developing a staff survey for primary care |
NHSE/I |
|
| Work to support higher attainment levels of overseas graduates through focusing on training and language needs | HEE | |
| The work of the BMA’s national BAME member forum | BMA | Ongoing |
| Programme of work to respond to all of the recommendations in Fair to refer, Gross Negligence Manslaughter, Caring for doctors, caring for patients and accelerating ED&I programme | GMC | |
| RCGP’s inequalities action plan | RCGP |
Membership
The sub-group will be formed of the following organisations
- Care Quality Commission (CQC)
- NHS England/Improvement (NHSE/I)
- General Medical Council (GMC)
- Nursing and Midwifery Council (NMC)
- Health Education England (HEE)
- NHSX
- Royal College of General Practitioners (RCGP)
- British Medical Association (BMA)
- Royal College of Nursing (RCN)
- NHS Race and Health Observatory
- Clinical Commissioners
- General Pharmaceutical Council
- General Optical Council
- General Dental Council
- Department of Health and Social Care
- Academic organisations
- Organisations representing ethnic minority providers/healthcare professionals.
Quorum and decision making
- The quorum for transaction of business shall be representation from a minimum of five organisations.
- Decision making will be inclusive as far as possible and by simple majority.
5. Frequency of meetings
- Meetings will be held every month for the first quarter of 2021/22, then frequency subject to review.
Secretariat
- The Chair is held for a period of three calendar months at a time, alternating between NHSE/I and CQC.
- The agenda for each meeting will be circulated in advance together with any supporting papers and will be distributed by the Chair. Any items to be placed on the agenda are to be sent to the Chair ahead of the meeting and accompanied by all relevant background papers.
- The Chair will provide support to record notes and action points of the sub-group meetings, including the recording of names of those present and in attendance. Notes and action points shall be circulated promptly to all members by the Chair.
Contributors
We would like to thank all those who contributed their time and expertise to this report, in particular Professor Aneez Esmail of the University of Manchester, the members of the sub-group of the Primary Care Quality Board, Dr Bola Owolabi, Director of Healthcare Inequalities, NHS England and Improvement and the members of our Expert Advisory Group:
- Olufemi Daramola, Christian Medical Fellowship
- Helen Davies, The Deep End Project
- Jane Ferguson, University of Manchester
- Shan Hussain, Doctors Association UK
- Shehla Imtiaz-Umer, British Islamic Medical Association
- Nadia Khalid, Muslim Doctors Association
- Anique Liv, Royal College of General Practitioners
- Ayiesha Malik, National Association of Sessional GPs
- Ore Odubiyi, BME Medics
- Kathy Smith, National Association of Sessional GPs
- Salman Waqar, British Islamic Medical Association
This print option will include all the text on this page.