Key findings
- Access to NHS dental care for all has been highlighted as an issue since long before the pandemic.
- At the start of the pandemic, routine NHS dental services paused, and then practices introduced enhanced infection prevention and control measures to help prevent the spread of COVID-19.
- The pandemic has compounded previous issues about access to dental services, as it has resulted in reduced capacity.
- There has been an increase in feedback from the public expressing difficulties in accessing dental care during the pandemic, which can have a strong impact on people’s general health and wellbeing.
- We have seen examples of dental providers adapting their practices well to respond to the pandemic.
- Although there were some examples of dental services working well with other health and care providers in a community, there were also difficulties that prevented people from receiving a prompt, joined-up experience of care.
Questions for the sector to address
- Listening to the views from the public on access: how will confidence be restored that access to NHS dental services is available for everyone?
- Access to urgent dental care: what measures need to be taken to prioritise and improve access to urgent dental care through NHS 111?
- Commissioning access: is there enough NHS dental capacity commissioned, and how will NHS policy leaders and commissioners deal with the demand to ensure those who are vulnerable and without a dentist have equality of access to NHS care?
- Access to oral and dental health care in a future system of integration: with a move to system working and joined-up working in a place, how will oral health be seen as an integral part, providing access to the right service, in the right place, first time?
Introduction
Like all health and care services, the COVID-19 pandemic has challenged how primary dental care is delivered. We carried out some analysis to improve our understanding of how dental practices have managed and supported people to access appropriate treatment during this time.
We analysed information from different sources, including feedback to CQC’s Give Feedback on Care service and to Healthwatch, and data from the NHS Business Services Authority around NHS dental activity. We combined this with analysis of what we have heard from 102 providers of dental care that we spoke to between January and March 2021. Where applicable, we have supported this analysis with the findings from two Provider Collaboration Reviews; the first looked at how providers worked together during the pandemic in 11 localities between July and August 2020, and the second in eight localities across England in October 2020.
This briefing brings together those findings to give a picture of dental access throughout the pandemic.
Challenges to dental practitioners from the pandemic
During the first wave of the pandemic in 2020, routine NHS dental services paused in the interest of patient and dental staff safety. Practices holding NHS contracts were supported by receiving payment for their full contract value, and were advised to provide advice, pain relief and antibiotics where appropriate, following telephone or online consultations with people. During this time the NHS established urgent dental centres or hubs across England, but it took some time before all of these became operational.
From June 2020, practices steadily restored services, while introducing enhanced infection prevention and control measures, such as using additional personal protective equipment, leaving fallow time between procedures, and carrying out more frequent deep cleaning.
Dental providers told us they had made changes to their existing practices and policies to help prevent the spread of COVID-19, but that these measures had reduced their capacity to provide services. Of the 102 dental practices in our sample, around half (46%) said that staff absences as a result of the pandemic had no impact on ensuring continued and safe access to care. However, a further 38% said staff absence had a low impact on ensuring continuity. Three practices we spoke to said that staff absence had a high impact on ensuring continued and safe access to care; some services used agency or locum staff to minimise the impact of staff absence on their ability to provide services.
Financial challenges were raised by some practices, relating to costs for changes to the physical environment, increased costs of heating bills (resulting from the need for extra ventilation) and clinical waste disposal.
Issues with access to dental care
Access to dental services
Access to NHS dental care for all has been highlighted as an issue since long before the spread of COVID-19, and there are clear signs that this has been compounded by the pandemic. Our Provider Collaboration Reviews showed that access to dental services during the early stages of the pandemic was a challenge for people. Urgent dental care hubs were specially established so that people could see a dentist in-person. Some places responded quickly as they had well-established relationships within the health and care system. In some areas, people struggled to get appointments and this had a knock-on effect for other urgent and emergency services, such as emergency departments. NHS 111 sometimes struggled to direct people to the right service and dental services that remained open found it difficult to meet the level of demand they faced.
Although the majority of feedback Healthwatch received about access to dental services expressed difficulties, some feedback to Healthwatch expressed gratitude for emergency dental care hubs and positive experiences of timely emergency care.
I had to make a few calls about a dental problem and after talking to two nurses and one dentist I was seen within a week. I waited in the car, they called me on my mobile, I was met by a nurse at the side door, given sanitiser for my hands and was offered a mask. The dentist was extremely thorough and explained the procedure in detail. Removal of a very decayed, very loose back tooth was painless and quick. Aftercare pack was explained, and I was given a number to call if I was worried about anything. Well done our NHS!
Experience reported to Healthwatch England
The impact of COVID-19 on the service available is clearly seen in our analysis of data from the NHS Business Services Authority on the total units of NHS dental activity (UDA) recorded. UDA provides a measure of how much NHS dental treatment has been delivered (with more complicated courses of treatment being made up of more units) – in 2020, this was 58% lower than it was in 2019. Activity was similar to the previous year between January to March 2020, but the impact of the pandemic and lockdown at the end of March 2020 meant that by April 2020, figures were 85% lower than they were in the same month in 2019 (figure 1). Activity levels fell to their lowest in May 2020, a reduction of 98% on the same month in 2019.
From June 2020, following the easing of lockdown, activity levels slowly started to increase and there were positive signs in the rate of recovery of urgent NHS treatments in the latter part of 2020. The latest data we reviewed for February 2021 showed that UDAs were still 40% below what they were in the same month in 2019. This is an expected consequence of the compliance with infection prevention and control, and public health, measures.
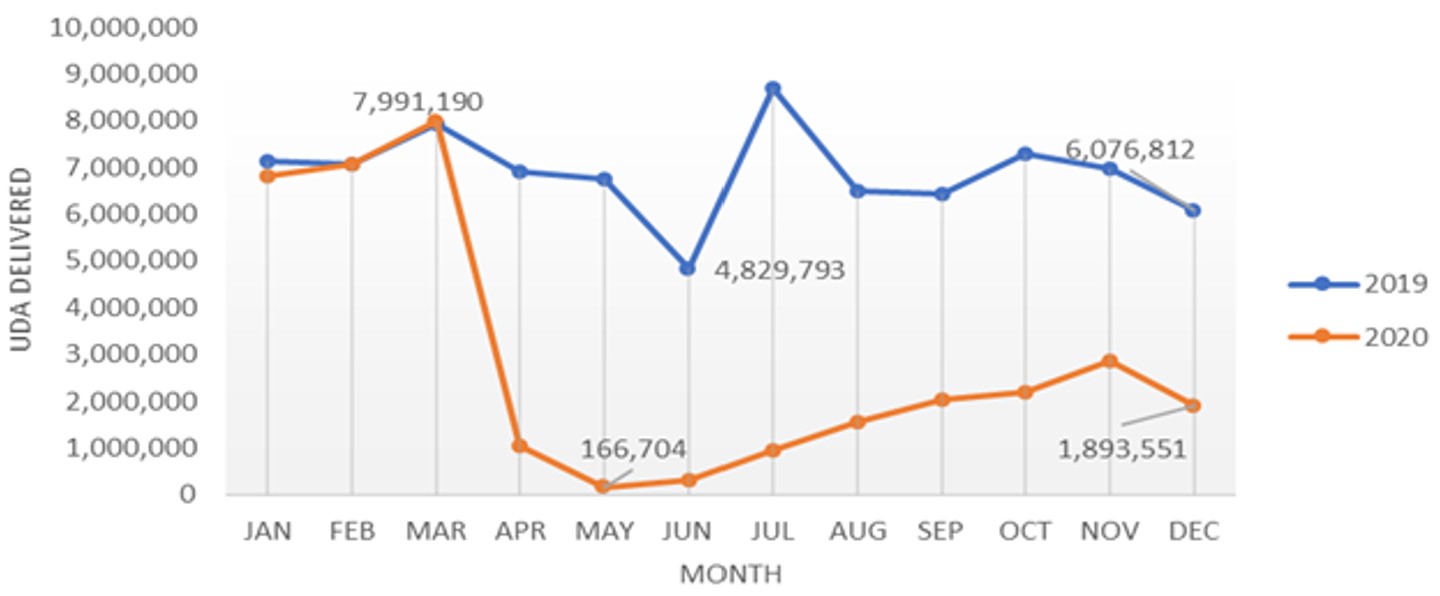
Source: NHS Business Services Authority (data supplied 24 March 2021. Data supplied by NHS BSA, analysis carried out by CQC).
Data from NHS England and NHS Improvement for the period March 2019 to February 2021 shows that there was dip in the percentage of calls NHS 111 triaged and recommended to dental services in March 2020, coinciding with the COVID-19 pandemic and the first lockdown. However, between March and May 2020 the percentage of these calls more than doubled from 3% to over 7% and remained above pre-pandemic levels over the rest of 2020 and into 2021, although figures are slowly reducing.
The increase in NHS 111 calls triaged to dental services since the onset of the pandemic suggests an increase in people who have not been able to access dental appointments locally and so have had to contact NHS 111.
Other data shows an increase in contact to NHS England and NHS Improvement from the public relating to dental services during the pandemic, the majority of which related to difficulty accessing dental care. At the pandemic’s onset, and with the temporary pause of NHS routine dental services from March 2020 to 8 June 2020, there was a drop in enquiries made to NHS England and NHS Improvement about dental practices. However, there was then a sharp increase, and by December 2020 the level of enquiries was three times what it was in December 2019 (figure 2). Also, there were five times more queries about access to dental services than there were queries about access to GP practices between September and December 2020.
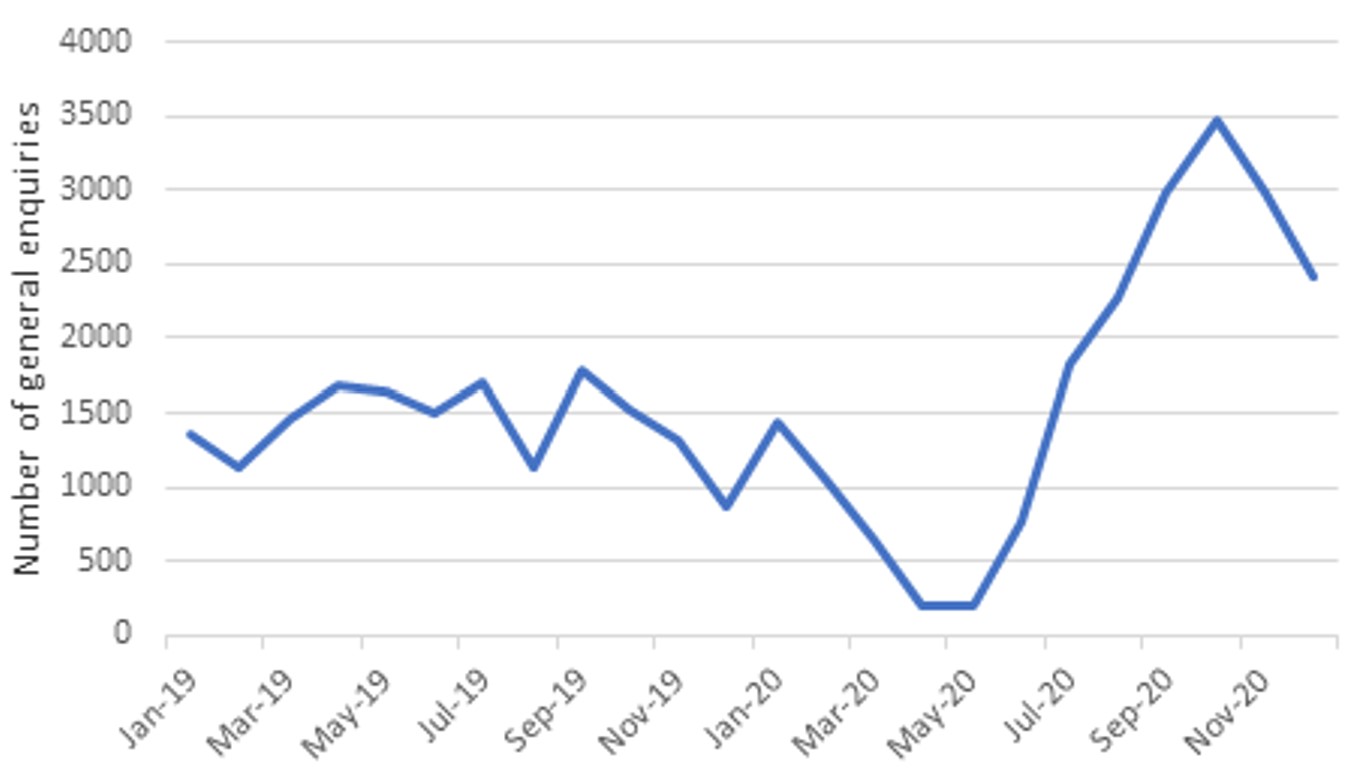
Source: NHS England and NHS Improvement: data as at January 2021
Impact on people
Access to NHS dentistry is one of the recurring issues that Healthwatch have reported on since 2013. However, the total volume of feedback from the public that Healthwatch received increased dramatically during the pandemic, with feedback regarding dentistry increasing at a much higher rate than any other area of health and social care. Issues around booking routine care, restarting treatment that began before the pandemic, and getting emergency treatment were common themes.
Across July to December 2020, more than seven in 10 people who contacted Healthwatch to share their experiences of NHS dentistry said they “found it difficult to access help and support when they needed it”. This resulted in people referring to an increased fear and anxiety about when they might be able to get an appointment, travelling long distances to access care, and at times experiencing debilitating pain and deterioration of their condition leading to treatment that could have been avoided.
One area highlighted by Healthwatch was that people were reporting that some dental practices were treating private patients but not NHS patients.
A lady called for advice in relation to COVID-19 dental access for her friend who had been up all night in agony. Her friend had been advised by her dentist that a root canal and a crown is needed but that ‘due to Coronavirus this is not available on the NHS and only available to you privately’, at a cost of over £1,000.
Experience reported to Healthwatch England
Issues with access and the difference between NHS and private treatment is somewhat reflected across the 102 dental locations we spoke to. Just under half (48%) were currently accepting both new NHS and private patients, while a further quarter said they were accepting only new private patients – although we did also hear examples of practices that were prioritising NHS patients, a specific contractual expectation set by the NHS to qualify for continuity of contract payments. However, 23% of locations said they were not accepting new NHS or private patients, which means that people who were not on existing dentists’ lists may have struggled to access care.
Delays for appointments for both routine treatment and exams as a result of the pandemic were more common for NHS patients than private patients. The difference in additional waiting times between NHS and private patients for routine exams was particularly clear, with nearly 54% of locations treating private patients saying there was no change in waiting times as a result of the pandemic, while only 45% of locations treating NHS patients said the same (figure 3).
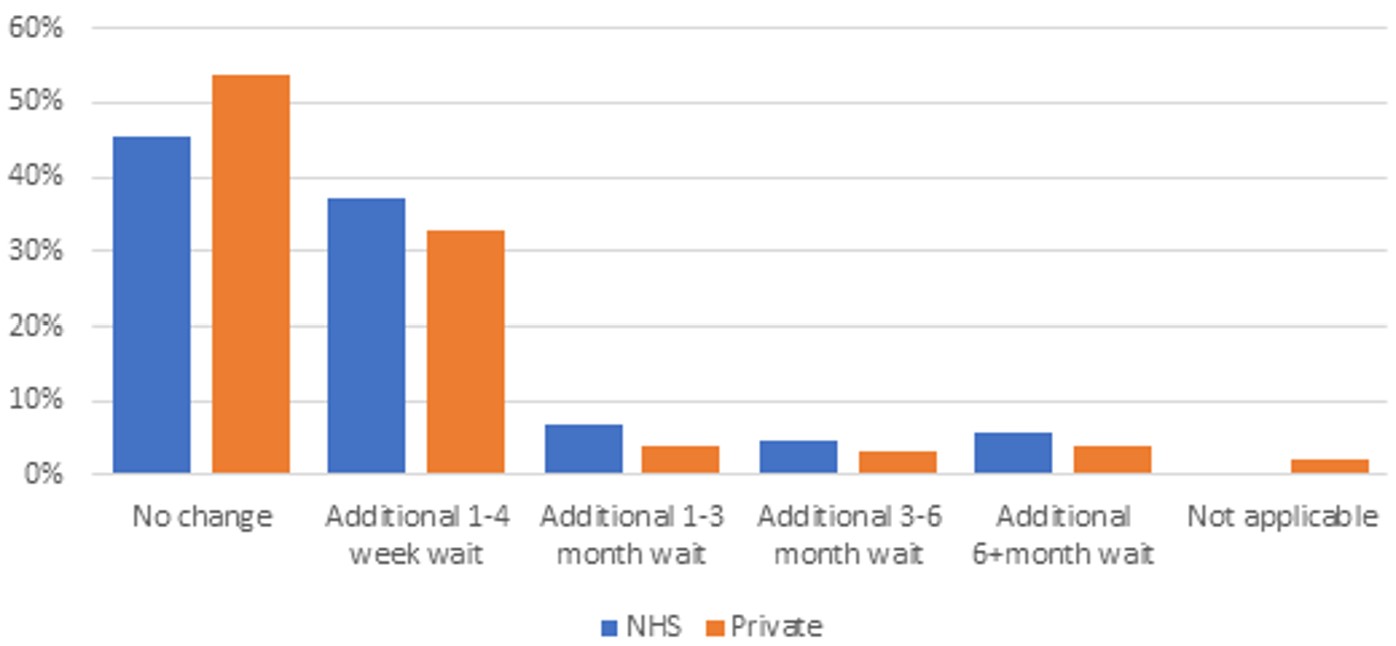
Source: CQC, January to March 2021 (NHS: n = 85; Private: n = 97).
There was a slight increase in feedback about accessing dental services to CQC via our Give Feedback on Care service, phone calls and social media between April and December 2020. Overall, over half of the approximately 750 pieces of feedback we received about dental services related to access.
Analysis of a sample of these pieces of feedback revealed that when people tried to access services, they often had to work hard to ensure they were seen, listened to, and that referrals went through. Urgent and emergency treatment was especially hard to access, and some people were told they had been ‘deregistered’ with their usual dentist and were unable to find help elsewhere, even though, as NHS England says, people do not need to register with a dentist. This raises questions about whether people who are less able to advocate for themselves could access care at all.
Reflecting on the feedback to Healthwatch above, the personal impact on people who did not have good access to services (across both dental and GP services) was sometimes significant, with people feeling abandoned, disrespected, frustrated, and sometimes in pain.
We called for an emergency dental appointment. They point blank refused to see us, and told us to call the emergency dentist. When we advised they were not seeing anyone, they told us they couldn't help.
Feedback to CQC's Give Feedback on Care service
Communications and engagement with people
Over three-quarters (77%) of the dental locations we spoke to said that multiple sources of information were available to support people to access services, including information on websites, on answerphones, or by email, text or social media. Nearly all locations said that information was up to date and told people how to access out-of-hours or urgent treatment.
Although several practices were highlighted by inspectors for providing a good amount of information on their websites, a quarter of locations had issues with information being accessible to different groups of people, including non-English speakers and those with other communication needs. A few practices did not have websites at all. These issues are supported by Healthwatch feedback, which talked of a lack of clear information, including from dental practices themselves, NHS 111, and the NHS ‘Find a dentist’ website.
Services also told us that some patients were reluctant to visit their dental practice during the pandemic and that they wanted to postpone their treatments until they felt safer to return. Practices described how they kept in regular contact with those people through phone calls and emails to ensure their condition did not deteriorate. One practice carried out an audit of attendance for check-ups, which indicated that people may be more confident to come for check-ups once they have been vaccinated.
Adapting practices during the pandemic
Staffing and scheduling
During both our discussions with the 102 dental locations and our Provider Collaboration Reviews, dental providers expressed pride in their staff, including their adaptability to new ways of working. Employees tended to feel supported by their employers to feel safe and have the skills they needed, with one practice organising "Regular updates and team learning and WhatsApp groups for the staff team, which has helped with improving each other’s mental health".
Most of the 102 dental locations we spoke to indicated that they supported staff to triage patients during the pandemic. For example, in services where the receptionists were responsible for triaging, the provider indicated that they were trained by nurses or clinicians. In some cases, senior staff monitored incoming calls and, in many cases, dentists were available for support if necessary.
We heard from practices that had also updated their continuity plans in response to the pandemic, for example to address how staff shortages might be managed or in response to an unexpected closure. Others told us about how they had updated their standard operating procedures as new guidance had emerged.
Some services reported offering additional hours in order to manage the number of people waiting for a service, including opening on Saturdays and extending hours during the week to as late as 8pm.
People could also be referred between sister practices, and we heard about some buddy arrangements between different providers, to take on each other’s patients in the event of a sudden closure.
Technology
Technology was used by dental providers to help them continue providing services during the pandemic.
One service described how they purchased an additional software licence to enable a staff member who was shielding to work from home and manage the waiting list. Another used an internet-based phone system that allows the practice to open up phone lines according to demand, and re-direct them to any staff working from home. Staff also have remote access to computers in the practice in case of homeworking or unexpected closure.
Many people were said to be happy with online or phone consultations, although some clinicians were hesitant about them due to privacy concerns and the additional difficulty in reaching an accurate diagnosis. We did note that a quarter of our sample of 102 dental locations did not enable appointments to be booked online or via email.
Supporting vulnerable groups
Although we have referenced above differences between NHS and private care, which could disproportionately affect low-income groups, as well as accessibility issues, our Provider Collaboration Reviews found that dental practices appeared to have a focus on supporting vulnerable groups during the pandemic. This was in line with the guidance from the Chief Dental Officer on the resumption of services. For example, they worked to meet the needs of people vulnerable to COVID-19 by giving them appointments at quieter times of day.
This was also reflected in our conversations with 102 dental locations. Alongside triaging systems, many told us they have a system, policy or process for assessing and then identifying vulnerable people. As well as those at greater risk from COVID-19, there were also systems for identifying people with other needs, for example resulting from a disability, physical or mental health condition, or neurodiversity, or children and adults made vulnerable by their circumstances, such as older people and cared-for children.
These groups were often given access to appointments with dentists or hygienists sooner or more frequently than others, or had their needs individually assessed and catered for, including referrals to other more suitable services if necessary. Some practices spoke about how people with higher clinical needs were proactively contacted to book appointments when practices reopened after the first lockdown.
Although most people were asked to attend appointments alone, people with learning disabilities could be accompanied. Extra-long appointments were provided for those who needed them (for example, people with learning disabilities, those with mental health conditions, people with autism and people with phobias about dentistry).
For people who were shielding or could not attend in person, a number of practices provided regular consultations online or by phone, or check-ins or wellbeing calls to help people maintain their oral and dental health. Some people at high risk of tooth decay, particularly children, were prescribed fluoride varnish following remote assessments.
System working
There is a mixed picture of working across services (system working) throughout our various sources of information.
Across the locations we spoke to, relationships with community pharmacies were most commonly reported as being positive and collaborative, followed by relationships with NHS 111, secondary care services and urgent dental centres. However, over a quarter of locations also described their relationships with urgent dental centres as being limited, inconsistent or non-existent.
Half of locations we spoke to responded ‘not applicable’ when asked about their relationships with care homes, and a further 32% said their relationships were limited, inconsistent or non-existent. Nearly a third of practices responded ‘not applicable’ when asked about their relationships with GPs and a further 26% said relationships were limited, inconsistent or non-existent.
Some of the 102 dental locations had been proactive in helping their system partners. For example, one location was a founding member of a local ‘cluster’ group, which brought together a range of dentists with a variety of skills, plus secondary and other care services to ensure a faster turnaround for people requiring secondary care treatments in the community.
However, we also heard about some challenges with referring people on to secondary care during the pandemic, for example orthodontic or oral surgery services. Dental providers described long waiting lists or delays, and referrals to specialists in centralised locations being difficult during lockdowns when travel was discouraged. Feedback to CQC through our Give Feedback on Care service spoke of the inability to access dental appointments, which led some people to seek help elsewhere, such as emergency departments, which places pressure on other parts of the health and social care system.
This also places a burden on people using services. In one Healthwatch case study, a patient was shuttled between their own registered dentist, NHS 111 and an emergency dentist and ended up having to go to an emergency department to receive treatment.
Our Provider Collaboration Reviews found that dental services were not always invited to be an integral part of the system for shared planning and system-wide governance. This resulted in services being left out of joined-up technology initiatives, including electronic prescribing services, and access to NHS email. Dental services also did not have access to summary care records, creating a barrier to people moving efficiently through the health and care system.
Read more...
Download the report
You can download a version of this report if you want to print or share it with your team.
Related news
You can also read our news story about the publication of this report:
Previous issue
You can read the issue of the report that we published in March. This issue looked at the impact of the pandemic on urgent and emergency services and the safe and effective use of medicines in NHS trusts.