North Yorkshire Council: local authority assessment
Downloads
Overall summary
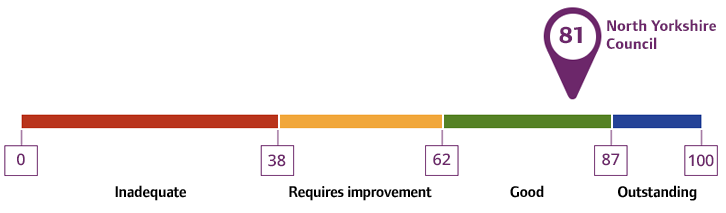
Local authority rating and score
Quality statement scores
Summary of people’s experiences
People generally felt happy with the care and support they received from North Yorkshire Council. They were able to find the advice and information they needed to make choices about their care. The support they received was well organised, and staff worked closely with them and each other to help people achieve their goals. Social workers kept in touch, and most people felt listened to and supported during the whole process.
People said they were treated with respect and their rights were protected. They were involved in making decisions during assessments and reviews, and their individual
characteristics such as age, disability, or background were recognised and considered in their care plans.
Many people were able to stay in their own homes for longer, through the care, support and equipment provided. They felt this helped them remain independent.
People said they felt safe using the services. They were helped to understand and manage any risks they faced. Data showed 73.69% of people receiving support felt safe, and 85.06% of carers felt the same. People had access to clear information about staying safe, what safeguarding meant, and what to do if they were worried about their own or someone else’s safety.
Most people had a smooth experience when moving between services. Staff worked hard to make sure these changes were handled as smoothly and supportively as possible.
Summary of strengths, areas for development and next steps
Senior leaders, managers, and staff in North Yorkshire were committed to strength-based approaches which helped people stay independent and delayed the need for formal services. Staff shared examples of supporting people’s independence, such as providing equipment so people could live safely at home with a focus on achieving positive outcomes.
The move to a unitary authority had improved coordination between the Health and Adult Services directorate and Housing, leading to better engagement and smoother processes. Extra-care housing was embedded across the county and had a clear, positive impact on people.
Restructuring within Health and Adult Services was taking place to focus resources more effectively, with staff engaged and enthusiastic about the changes. Governance and risk management were strong, supported by good data which was used to track progress. Council members were well-informed and supportive of adult social care, with good scrutiny arrangements in place.
The local authority presented a confident, values-led approach to equity which was both practical and embedded. It included lived experience, intersectionality, and inclusive language, with clear commitment to co-production and continuous improvement. The strategy avoided tokenism by linking equity to governance, workforce development, and service design, whilst challenging structural barriers. The local authority’s strength lay in making equity everyone's business, anchored in accountability, compassion, and measurable impact.
Plans for a North Yorkshire Health Collaborative, a formal section 75 Joint Committee between the largest Integrated Care Board and the local authority, with wider NHS, Voluntary and Community sector and care sector involvement, were being finalised to go live in July 2025, supported by leadership investment. Partnership working across services and with voluntary and community groups was strong, and co-production with people with lived experience helped shape services. The local authority used local data well to understand needs and address inequalities. It worked closely with partners to plan for current and future demand.
Safeguarding was a clear priority. Risks were well understood, incidents were dealt with quickly, and learning from reviews was used to improve practice. The Emergency Duty Team played a key role in managing urgent risks.
People had access to safe, high-quality care services, including those registered with the Care Quality Commission. Waiting lists were managed with oversight to ensure those most at risk were prioritised. Carers who had an assessment generally found it helpful and became more aware of available support. Some people used services outside of the county, but efforts were underway to expand local options. Out-of-county placements were monitored, and many had achieved good outcomes.
The local authority took a proactive role in developing services. There were many ongoing and planned projects, including extra-care housing, dementia care, and replacing outdated council-run care home buildings with up to 5 new Care and Support Hubs. However, issues remained around access to mental health beds and home care in rural areas, though pilot schemes were in place to address this.
Intermediate care and reablement services helped people regain independence quickly, supported by a strong referral process. The introduction of the new occupational therapy assistant roles had reduced waiting times. Leaders aimed to grow preventive services like Community Anchors and Care and Support Hubs and increase support for working-age adults with mental health needs, helping more people live independently.
Transitions, particularly of children to adulthood were handled with care. Improvements had been made to hospital discharges through joint working and models such as ‘discharge to assess,’ although some challenges persisted, such as shortages in specialist residential and nursing services for people with complex needs and due to pressures with waiting lists there are people waiting for assessments.
Staff were very positive and felt well supported, with a dynamic learning culture where learning, improvement and innovation was driven by curiosity, reflection, and collaboration. There was a strong visible and approachable leadership team who understood the challenges of frontline work.