Contents
- What the draft quality of life framework is
- Section 1: Is there a planned programme for each person that focuses on their quality of life?
- Section 2: Are the planned programme components relevant to each person's needs?
- Section 3: Are components of each person's support programme being delivered with fidelity at the right level of intensity?
- Section 4: Is there a balance of programme components and are support plans for each person coherent across settings and over time?
Delivering support that maximises the quality of life for people with learning disabilities experiencing emotional distress
Building the right support (2015) is the national plan for services for people with a learning disability and/or autism. It states:
“Children, young people and adults with a learning disability and/or autism have the right to the same opportunities as anyone else to live satisfying and valued lives, and to be treated with dignity and respect. They should have a home within their community, be able to develop and maintain relationships, and get the support they need to live healthy, safe and rewarding lives.”
We produced this draft quality of life framework with the PBS Academy. The draft framework was developed as an important first step in setting out an improved approach for evaluating the quality and effectiveness of service provision from the perspective of people using services.
The draft framework was then used as a basis for developing the quality of life tool we have been piloting as part of our commitment to improving how we regulate services for people with a learning disability and autistic people. We have written more about this in a recent blog post.
CQC and the PBS Academy acknowledge The Warwick ESRC Impact Acceleration Account for funding the development of these resources, both the draft framework and the tool being piloted. Thanks also to CEDAR, University of Warwick, for administering the project.




What the draft quality of life framework is
These questions should guide any assessment, audit and development of services to support people with learning disabilities:
- Who are the people the service is delivering support to?
- What are their needs and aspirations?
- Is the service meeting those needs and aspirations?
The quality of Life framework provides a structured and logical set of questions our inspectors might ask and that service providers should be asking themselves. They help us understand whether the service is meeting the needs and aspirations of the people it is supporting. It points to potential sources of evidence with guidance about how to find the answers.
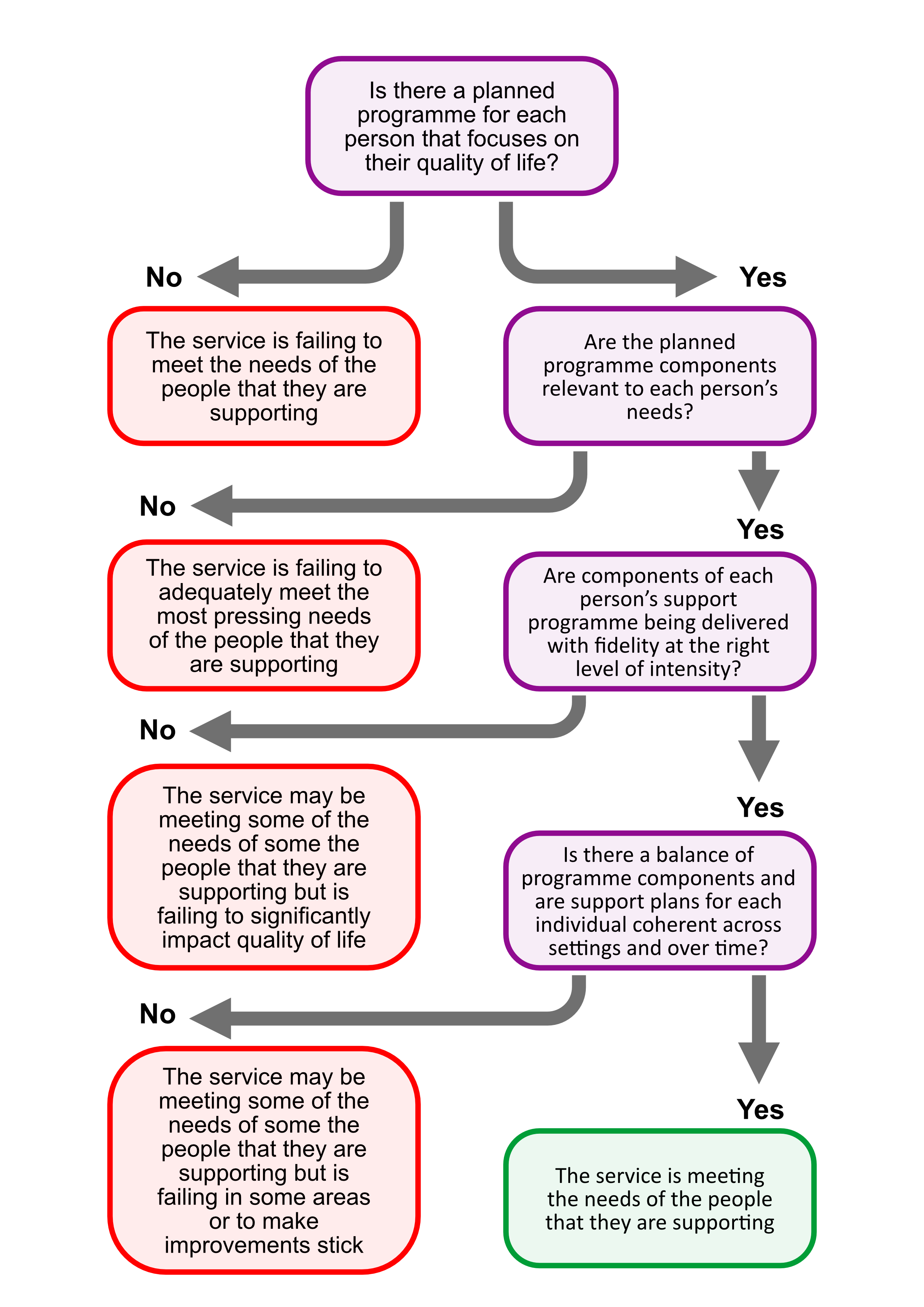
Is there a planned programme for each person that focuses on their quality of life?
If no: The service is failing to meet the needs of the people that they are supporting.
If yes: Are the planned programme components relevant to each person’s needs?
If no: The service is failing to adequately meet the most pressing needs of the people that they are supporting.
If yes: Are components of each person’s support programme being delivered with fidelity at the right level of intensity?
If no: The service may be meeting some of the needs of some the people that they are supporting but is failing to significantly impact quality of life.
If yes: Is there a balance of programme components and are support plans for each individual coherent across settings and over time?
If no: The service may be meeting some of the needs of some the people that they are supporting but is failing in some areas or to make improvements stick.
If yes: The service is meeting the needs of the people that they are supporting.
Collecting evidence
We recommend that anyone evaluating the quality and effectiveness of service provision participates fully in all these three areas of obtaining evidence. This allows you to:
- consider multiple perspectives
- challenge evidence across methods for consistency
- pool evidence and corroborate and agree it.
1. Observation
There are two types of observation:
- participatory: spending time with people in structured interactions (addressing specific questions) or informally (assessing a range of matters more broadly).
- non-participatory: 'fly on the wall' observation. It depends on having no interaction with the people being observed and as little impact as possible on what happens around them. This observation may be quantitative (for example, counting interactions according to a pre-defined criterion), or qualitative (for example, a narrative account of events as they occur). You can also record information using a checklist or rating scale at the time or soon after an observation has been concluded.
There are two methods for collecting information:
- direct observation: an observer is present in the environment to record their observations as they occur.
- indirect observation: someone collects information on the observer's behalf. For example, a member of staff or an individual receiving services.
2. Interview
Interview is useful for learning about the beliefs, attitudes, and experiences of staff and, where possible, gaining information on the perspectives of people receiving services. There are three main types of interview you may use in combination during an evaluation of positive behavioural support. These are:
- open-ended and informal: useful for discovery and formulating areas for further consideration.
- semi-structured: following a pre-determined framework, but flexible enough to explore some areas in depth and others superficially.
- structured: asking questions and recording responses in a prescribed manner, useful when a high level of precision is required.
3. Document review
A provider's policies and value statements should be reflected in the care being provided. This can be considered in three aspects:
1. Provider or organisational policies and information
Review of:
- the CQC statement of purpose of service and the provider's relevant value statements to establish the model of care being provided
- all whistleblowing, complaints and concerns, and other data in relation to the service.
2. Health and care plans
People's care treatment and support plans should reflect their sensory, cognitive and functioning needs.
3. Documentation relating to support for people at risk of behaviours that challenge:
- formal assessment of skills, communication, mental health status, physical and psychological health and well-being, psychiatric status, sensory and physical impairment, or trauma.
- care plans with measurable goals that are time-bound.
- person-centred plans that are aspirational, time-bound, and measurable.
- functional assessment report that
- defines behaviour
- specifies its occurrence (rate, duration, intensity)
- delineates physical, psychological, and sensory issues (from above)
- describes learning history
- reveals current context (antecedent motivative and discriminative properties)
- identifies maintaining factors (reinforcement - selection by consequences - and respondents)
- provides an analysis and formulated hypothesis.
- Function-based multi-component intervention plan that synthesises information from assessments and specifies actions designed to change the context in which behaviour has occurred in line with the stated hypothesis. Each plan should clearly state:
- targets for behaviour change and a time boundary
- a measurement system
- actions to enhance quality of life and prevent behaviour from occurring
- skills to be taught
- behaviour to replace challenging behaviour
- focused intervention
- reactive management strategies
- staff and carer training needs and supports.
- Behaviour support plan: a brief easy read guideline to help staff know how to support a person including recording for focused support.
- Monitoring and evaluation:
- data that describe a baseline (before change was introduced)
- the effects of change
- evidence that further change is or is not made in the light of those data.
Corroboration
Information obtained from observation, document review and interviews should be reviewed, discussed, and analysed to form a consistent narrative (storyline). Inconsistencies should be resolved, strengths and weakness in practice identified, for a service delivery plan with measurable development targets.
Section 1: Is there a planned programme for each person that focuses on their quality of life?
Does each person receiving care in the settings have a planned programme of support?
It should be clear that all the key elements, 'ingredients', that you would expect are present in a planned programme that focuses on quality of life. (See PBS Competence Framework "Creating high quality care and support environments".)
1. Is the environment appealing and does it meet people's sensory and physical needs - and is the culture kind, caring and nurturing?
Key questions: safe, caring, well-led
What might you see?
A living environment that you would be happy to live in yourself:
- appealing physical environment: sympathetic to the sensory and physical preferences of all people within the service
- empathetic social environment: staff are warm, appropriate, respectful, and positive towards the people they support and their families
- dignified interactive environment: staff are nurturing in the care and support to the persons they are working as rather than 'over-protective'.
A living environment that accommodates the needs of each person being supported. It provides options for peace and quiet and communal areas for socialising.
Staff consistently support individuals to engage and to communicate. They use non-verbal communication and communication aids if necessary.
Evidence that staff are noticing and responding to people's individual ways of communicating.
What might you hear?
Staff speak positively about their expectations for the people they support both in the present and for their longer-term aspirations and goals (direction of travel). This is reflected in day-to-day activities with staff ensuring that they can and do participate in all areas of their lives. Staff ensure support helps people to meet their longer-term goals.
The person and their family speak positively about all aspects of where they live.
What to look for in documentation
A statement of values that underpins the service. Evidence that the organisational culture, leadership, and infrastructure supports this.
Individualised assessments for each person (for example, by a speech and language therapist). These should outline communication needs and preferences and include an agreed plan.
Evidence that all staff use these individualised assessments consistently.
Red flags:
- Over-protective care: doing things for people because it seems kind to do so rather than encouraging them to do things for themselves. This could make people less skilled and independent.
- Avoiding involving people in activities due to perceived risks. For example, staff say they cannot include someone because their behaviours would be a danger to others.
- An unsuitable physical environment offering little flexibility to accommodate individual needs. There are cases where people being supported are having to move for their safety because someone is distressed.
- Communication support is provided by only one professional (for example, a speech and language therapist). Or evidence that all support staff cannot assess or support communication.
- Staff do not know the communication plan. Or they do not have the right knowledge or tools to be able to use it (for example, access to PECS symbols).
2. Do staff know the people they are supporting including their health and wellbeing needs?
Key questions: safe, effective, caring, well-led
What might you see?
People engage in activities they clearly enjoy or have expressed a desire to take part in. Staff organise activities for each person based on an understanding of what is important to them, their existing talents, skill set and knowledge, and what they prefer to do with their time. Activities also respect each person's religious (including their preferred place of worship), cultural, political, sexual, and other diverse needs.
Staff demonstrate a shared understanding of what wellbeing means to each person, by creating a daily routine that maximises their wellbeing.
Staff encourage a healthy lifestyle while respecting a person's right to live the lifestyle they choose. They attempt to incorporate healthy choices as much as possible into daily routines.
Staff teach new skills based on what has been agreed for an individual's personal development and growth. Skills teaching takes into consideration how the person would naturally perform, or would prefer to perform, that skill. (For example, when teaching someone to iron a shirt, start with sleeves if that is how they prefer it).
Each person has an active role in monitoring their health and wellbeing. Staff encourage and support them to achieve this.
What might you hear?
Staff talk knowledgeably about people's preferred activities and items, ambitions, likes and desires. This includes their life history and religious, cultural, political, sexual, and other diverse needs. Staff show a desire to continue learning about the person and adapting to new activities and preferences they may develop over time. This includes them deciding they do not enjoy an activity anymore).
People and their families talk about how well staff know them and how their needs are being met.
What to look for in documentation
In each person's daily schedule there is evidence that the chosen activities are based on what that person prefers and likes to do with their time.
An up-to-date health and wellbeing plan for each person. Records show they are registered with a GP and have an annual health check.
Each person's psychological needs are noted alongside medical needs in their health and wellbeing plan. This includes information about:
- their health needs and how to manage them
- medications
- signs to look out for that could indicate physical and mental health and wellbeing may be deteriorating.
Comprehensive records are kept in the service setting for each person. These include medication records, history of doctor's visits and health care procedures.
Red flags:
- No access to external health professionals outside of the service setting. This could lead to limited community access and engagement. It may increase the likelihood of a closed culture.
3. Are people engaged in meaningful activities and relationships?
Key questions: effective, responsive, well-led
What might you see?
People taking part in a range of relevant and age-appropriate meaningful activities throughout the day:
- around the home or unit (for example household chores, education, gardening, social activities)
- in the local community (shopping, leisure, education, work, social activities).
Staff support people to actively engage in these activities, rather than merely participating.
Staff:
- support people to do things for themselves as much as possible (including basic self-care tasks such as eating, wiping their face, serving their food)
- 'hold back' and allow the person to attempt to do the task or activity themselves
- are prepared to provide appropriate support to help complete a task or activity.
What might you hear?
People communicate (using their preferred method) when they will next visit their family and friends, and when in the week or day they would prefer to visit.
People, their families and staff talk about the activities they take part in – what they are doing, going to do, and have done.
What to look for in documentation
Participation indexes, or similar, noting the number of times each person has been able to take part in social activities out in the local community.
Records of dates when family and friends have visited, or when the person has visited them. Evidence that future visits are scheduled, even if preliminary, so that the knows when they will next have contact with their family and friends.
Support plans take account of people's preferences and the activities they enjoy.
Red flags:
- No record of participating in activities outside of the home or unit setting.
- No record of family or friends' visits (if appropriate to that person).
- Staff do not encourage independence when completing tasks. Staff do not appear enthusiastic or encourage engagement from everyone when taking part in tasks or activities.
4. Are staff supporting people to experience real choice and control?
Key questions: effective, responsive, well-led
What might you see?
Staff offer choices of activities to each person based on their known preferred activities. Staff present these choices so the person cannot use a learned response to pick (for example, the person always chooses the first option regardless of what it is) or use closed questions.
People exercise control over how activities unfold when they are taking part. For example, the order they do things and how long they do them for. Staff are flexible in the moment to what that person wants, with back-up activities in case that person wants to cut the activity short.
People choose when family and friends visit and communicate this in the way that suits them.
Evidence of people having chosen how their living quarters look (for example, how their room is decorated, at least for soft-furnishings and their own personal possessions).
If people request activities, or a particular food, that is not available to them at that time, staff respond to the request and help the person to plan for the future.
What might you hear?
Staff speak about how they support people to solve problems independently when faced with issues in their daily schedule, such as a preferred activity being cancelled.
People and their families talk about the choices they make or have made and how staff support these.
What to look for in documentation
Behaviour support plans note each person's preferences and preferred communication style.
Behaviour support plans include skills teaching to help people make informed choices where necessary.
Red flags:
- Staff dismiss requests made by people in terms of activities or particular foods without good reason.
- There is no evidence people have choice in how their day unfolds, or what activities they would like to take part in.
5. Are staff promoting a safe, consistent, and predictable atmosphere that meets people's individual needs?
Key questions: safe, caring, responsive
What might you see?
There is support - for example visual schedules to help people predict what is going to happen at least over the next few hours. This support should relate to what is actually going on at that time. If not, there should be a reasonable explanation why they are not aligned (for example, someone is ill, or the person requested to do a different activity last minute).
Staff increase and encourage people to plan their next day or week, to further support choice and control over their time. This should be appropriate for that person in terms of structure and planning (some only like to plan one day ahead of time, others a full week ahead).
Staff support people to come up with alternative solutions when unscheduled changes arise.
Staff continuously and dynamically assess risks within an activity or situation.
What might you hear?
Staff talk knowledgeably about the process of risk assessment. They understand how important it is to discuss with the person and relevant stakeholders to determine whether:
- the risk level for a new activity is acceptable
- adaptations can be made, especially if this new activity is deemed high-risk.
Family members and staff talk about the importance of visual schedules and how they use them to support people.
What to look for in documentation
The supports in place, such as visual schedules, are individualised for each person. Each person has their routine and their plan reflected upon their own likes and desires; not just the same plan or schedule for everyone.
Plans show evidence of a positive risk-taking strategy. Risks are identified and minimised rather than avoided all together, so a person can still do an activity that is important to them.
Records of up-to-date and relevant risk assessments relating to the service building and environment are on-site and available for all staff. Evidence that these are updated regularly and in line with changes to the building or environment.
Red flags:
- There is no evidence of risk assessments for the service building and environment.
- There is no evidence of risk assessments for activities that people may take part in, especially if these activities are deemed high-risk.
- There is no structure to a person's day, and that person does not know what will happen next over the next few hours.
6. Are complex needs and behaviours that challenge being supported effectively?
Key questions: safe, effective, caring, responsive
What might you see?
Staff use proactive strategies successfully to reduce the frequency and severity of challenging behaviour. For example, teaching skills to reduce the likelihood of behaviours that challenge, planning enjoyable and fulfilling activities and offering choice.
Staff are vigilant, watching people's reactions, paying attention to their non-verbal communication. They quickly identify if someone is becoming over-aroused, upset, frustrated, or withdrawn and act to ameliorate the situation.
Staff support the person after an occurrence of behaviour that challenges follow the protocol set out in the person's behaviour support plan.
Staff are aware when a person may be distressed. The absence of any behaviours that challenge may also indicate that a person is distressed (for example, freezing).
What might you hear?
Staff have a clear understanding of what behaviours that challenge look like for each person and explain this to others.
Staff describe the function of behaviours for each person and why they keep happening.
Staff describe the procedure for how the functional behaviour assessment has been conducted and by whom.
The person and family carers talk about how they have contributed to the functional assessment and the development of the behaviour support plan.
What to look for in documentation
There is a functional behaviour assessment to identify the function of the behaviours that challenge for each person.
In the functional behaviour assessment, there is a clear description of the function of the behaviour (for example, escape, attention, tangibles and sensory). These are explained and supported by examples.
Each person who may be at risk of behaviours that challenge has a behaviour support plan.
The behaviour support plan for each person:
- clearly reflects their functional behaviour assessment
- contains accurate and detailed information about the person's behaviour, including:
- a clear description
- early warning signs and triggers that make it likely to occur
- appropriate strategies for proactive support to enhance quality of life (for example teaching skills, reducing the likelihood of behaviours that challenge, planning activities that are enjoyable and fulfilling for that person, offering choice etc)
- reactive strategies for if behaviour that challenges occurs.
Red flags:
- Staff use the same strategies with every person they support.
- An inability to recognise that there is a wide spectrum of behaviours that may not be 'physically challenging' but could put people or those around them at risk or adversely impact their quality of life. For example, if a person 'freezes' when they need to be able to move, such as during a fire alarm.
- Behaviour support plans:
- show no evidence of being based on a functional assessment of the individual's behaviours, skills, preferences, etc.
- do not include teaching skills, targets and strategies in a way that is meaningful to and owned by the person
- are not in line with the assessed function
- An indication that support staff do not have a role in understanding behaviour that challenges. Instead, they think a specific behavioural team or individual is responsible for understanding, assessing, and supporting behaviour.
- A lack of understanding that it is essential to involve people in their plans as much as possible in meaningful ways.
- Staff talking about people, rather than their behaviour, as challenging. Or they use terms that devalue the person (for example, 'kicking off', being 'naughty').
7. Is there a clear commitment to minimising the use of restrictive interventions including restraint, and only using it as a last resort?
Key questions: safe, caring, responsive, well-Led
What might you see?
The service only uses restrictive interventions including restraint as a last resort.
If staff use any unplanned restrictive strategies, this triggers an immediate review of the person's support. It also triggers the implementation of their behaviour support plan.
Evidence that a debriefing of staff has taken place after any incident involving the use of a restrictive intervention.
Evidence that the family carer or advocate is informed of any restrictive interventions.
What might you hear?
Staff speak knowledgeably about restrictive interventions and say restrictive practice should only occur as a last resort. Staff discuss the techniques they use that could help them reduce their use of restrictive interventions with the people they are working with.
Staff give examples of when they have had a debrief, how this has supported them, and the changes that have been made after the debrief (in practice as well as reflected in the behaviour support plan).
The person talks about how they have been supported after the use of a restrictive intervention and their own thoughts about this.
The family carer or advocate (where appropriate) talks about any restrictive intervention that has been used and the contribution they have made to any subsequent changes in the support given to the person.
What to look for in documentation
There is evidence of every time restrictive interventions have been used, including restraint. Records and evidence should be comprehensive. They should describe exactly how the incident unfolded.
The service's statement of values should clearly outline that using restrictive interventions, including restraint, is always a last resort.
There should be a clear restrictive interventions reduction plan.
Red flags:
- There is no, or poor, recording and monitoring of the use of restrictive interventions. There is no evidence of reflective practice and debriefs after the use of any restraint (for example, physical, chemical, or mechanical).
- There is no evidence that a clear restrictive production plan is in place or referred to.
- Staff say there is no alternative to restrictive interventions and push for the use of restrictive interventions first.
- A lack of awareness that practices such as limiting people to specific areas (for example, their bedroom) or blocking access or exits constitutes restrictive practices.
8. Is there effective practice leadership and support for service staff wellbeing?
Key questions: caring, well-led
What might you see?
Practice leadership, used to support staff and promote good practice is in evidence. Managers are leading from the front, working directly with the people the service supports and coaching and mentoring in situ.
Staffing elements, such as numbers, skills, deployment, and staff ratios appear to be well managed in line with the needs of each person and groups. This enables a safe and enjoyable working environment for staff and the people they support.
Evidence of a management culture that values and prioritises opportunities for staff to reflect, question and discuss their working practices and the impact these can have on the wellbeing of the people they support and behaviours that challenge.
What might you hear?
Staff speak positively about being able to discuss matters of concern with management, as well as reflect on their own practice without fear of reprisal.
All staff provide feedback to one identified lead, indicating everyone knows what to do and how to behave. In this respect, there is a culture of improvement.
Staff say they feel safe within the working environment and discuss the ways that they are encouraged by management to look after their own health and wellbeing.
If staff are required to work alone with one person for the entire day, senior staff or management provide a good rationale for why this is. For example, the service believes that pairing staff with a person for the entire day maintains consistency.
Managers and senior staff speak knowledgably about the most recent and relevant legislation and guidance appropriate to the individual type of service and characteristics of people using it.
People and their families talk warmly about the staff that support them and clearly have developed good personal relationships over time.
What to look for in documentation
A personal development plan for each member of staff that is compatible with the needs of the person or people they are supporting.
A recruitment policy that helps identify potential candidates who have a person-centred mindset or values.
Red flags:
- Staff say or indicate non-verbally that they do not feel safe in the working environment. They say they cannot talk about these concerns to senior management.
- A high staff turnover ratio or use of agency staff.
- Poor practice or negative talk goes unchallenged.
9. Is there an effective programme of service staff training and is there evidence of this being embedded into practice?
Key question: well-led
What might you see?
Evidence of on-the-job supervision and training.
Acknowledgement and celebration by senior staff of good practice demonstrated by any member of staff.
Evidence that the service encourages staff to understand and comply with relevant legislation.
Staff work as a team and support each other. They encourage reflective practice – for example, supporting others to improve their working practice.
What might you hear?
Staff describe their learning and personal development through training and ongoing supervision. They describe the impact this has on their practice.
Staff discuss how they would ask their manager or senior staff for training in areas they are interested in. For example, positive behaviour support or active support.
Staff speak positively about an organisational culture that encourages reflective practice and continual professional development.
Staff speak knowledgeably about relevant legislation and guidance. They can apply their knowledge to their practice at a level that's appropriate to their role.
What to look for in documentation
A workforce development plan based on a training needs audit.
Records of staff supervision with senior staff or managers. These include details of job coaching and onsite training given to less experienced staff.
There are records of relevant qualifications staff have obtained. There are training and development plans for each staff member, in line with training criteria essential to the service.
Evidence of staff receiving regular training associated with reactive strategies including physical interventions, manual handling, behaviour skills training, or related and communication methods (for example, PECS and Makaton).
Red flags:
- No records of staff training. Little evidence of continuous professional development in staff records.
- Staff records indicate staff are underqualified for their roles and they require further training. This is particularly noticeable for training in physical interventions and manual handling.
- No clear procedures for supporting team working, peer support or reflective practice. Or no recognition of the importance of these elements for providing good, consistent support.
Section 2: Are the planned programme components relevant to each person's needs?
It should be clear from observations, discussions, and documentation that all of the 'right ingredients' for a person's support plan are being used. The right stakeholders should be helping to develop them (ref PBS Competence Framework 'Developing and Implementing a Behaviour Support Plan (BSP)').
10. Has each person's programme been developed to meet their current needs and preferences as well as longer-term aspirations?
Key questions: effective, responsive
What might you see?
Evidence that the person's support includes ways to give them more autonomy. This means enabling them to make their own decisions and exercise self-control. Staff enable this by encouraging people to make their own decisions and have control over how they spend their time.
Evidence that the person is learning skills that help meet their current and longer-term needs.
What might you hear?
Staff talk about how they identify targets for skills teaching based on:
- what's important to the person
- developing their independence
- alternative ways of fulfilling the function of any behaviours that challenge.
Staff discuss ways to ensure targets are meaningful to the person and have clear goals.
People and their families talk about the goals that are important to them and these are reflected in their daily activities.
What to look for in documentation
The behavioural support programme for each person sets out their current needs and future goals, and there is a clear pathway between the two.
Evidence of a range of assessments conducted for each person including:
- preference assessments (likes and desires)
- functional assessments to identify the function of any behaviour that challenges
- assessment of skills and goals that inform skills teaching targets
- sensory assessments
- medical and psychological wellbeing assessments.
Evidence that these assessments have been used to develop support for the person.
Evidence that these assessments have been repeated, if necessary, for each person in line with changes in the person's preferences or circumstances.
Each person's programme includes detailed advice or methods about how to meet their communication needs.
Red flags:
- There is no evidence of future planning or consideration of the person's longer-term aspirations.
- There is no evidence the person has the opportunity to make choices during a typical day
11. Do staff monitor and evaluate each person's outcomes meaningfully and review their support plan, adapting it where necessary?
Key questions: effective, responsive
What might you see?
Data is collected and used to update support plans where relevant. For example, if skill-acquisition data shows that a person has successfully learnt a targeted skill, stakeholders jointly decide on a new target.
Staff regularly give feedback to management, other staff, family, and friends about the support the person is receiving and their wellbeing.
Staff ensure this feedback is used to adapt existing plans and procedures.
What might you hear?
Staff talk positively about the progress people have made towards their goals. They describe how, as a team, they ensure that the support they give evolves so it continues to meet each person's changing needs.
What to look for in documentation
The service keeps records about outcomes such as quality of life, communication, skills teaching, engagement in meaningful activity and behaviours that challenge.
Evidence that support plans are updated and adjusted to reflect what the service has recorded.
Red flags:
- No records are kept on outcomes, or outcomes are rarely recorded, and the records do not inform current behaviour protocols or support plans.
- There is no evidence of support plans having been updated. Or if they have been, they include the same protocols or targets as previous versions.
12. Are relevant stakeholders (including the person and their family) involved in the development of the person's support plan in a meaningful way?
Key questions: caring, responsive
What might you see?
Evidence stakeholders - such as guardians or carers - are involved in the development of the person's support plan and kept informed if it needs to change.
Evidence that the organisation encourages families and carers to be involved in the decision making, policy formation, recruitment and shaping aspects of service development.
Evidence that staff and organisations provide the appropriate support for people who may not be able to self-advocate, and signpost to independent advocacy services if required.
Staff support people in a way that empowers them to make decisions for themselves. They do not assume that people who are unable to self-advocate in one area of their life also lack capacity to make decisions in other aspects of their life. For example, a person may lack capacity to make complex financial issues decisions. But they may still have the capacity to decide what new skills they would like to learn.
What might you hear?
Stakeholders (including the person being supported and their family) describe how they have contributed to the development of the person's support plan.
Stakeholders (including the person being supported) speak positively about how they can give feedback to the service, and how this feedback is used to improve their support and celebrate good practice.
What to look for in documentation
Evidence that stakeholders (including the persons who use the service) are involved in shaping the organisation. For example, stakeholders may be on recruitment panels or steering groups, or give feedback on policy. Evidence of this may be shown through participation records or through plans to increase the use of stakeholder input into the service.
Evidence that the person themselves is supported to be involved in all aspects of the support they receive, in whatever way they can. For example, records of the person taking part in meetings and reviews, or having their preference assessed and respected.
Evidence of a review for each person in terms of mental capacity, including capacity to consent. If relevant, there should be information about the independent advocate for every person who needs one.
Red flags:
- No involvement of multiple stakeholders within the development of people's support plans or behaviour support plans.
- No involvement of family members, guardians, or carers in the continuous development of the service (for example staffing and recruitment).
- A suggestion that supporting the emotional wellbeing of stakeholders (and in particular, family and carers) is not within the remit of the service or is not considered by the service.
Section 3: Are components of each person's support programme being delivered with fidelity at the right level of intensity?
It should be clear from observations, discussions, and documentation that components of people's support plans are being implemented at the correct dose and intensity (ref PBS Competence Framework 'Developing and Implementing a Behaviour Support Plan (BSP)').
13. Does each person's programme offer sufficiently intensive learning opportunities to help them acquire skills?
Key questions: effective, responsive, caring, well-led
What might you see?
People continuously learn new skills that are important to them (that meet identified goals). They are appropriate to the person's level of cognitive ability. But they also 'challenge' the person and build on their current skills level to help them achieve their potential.
People receive new skills teaching regularly, delivered consistently from all staff members. The teaching is sufficiently intensive and appropriate for the skill being taught. For example, horse riding might be appropriate once a week but stacking the dishwasher might be daily.
Skills are taught in a person-centred way. This means they're taught according to each person's preferences. For example, cutting crusts off bread when making a sandwich, if that is the way the person prefers. These skill targets are also in line with the person's priorities.
People are engaged consistently throughout the day and in all activities they take part in.
What might you hear?
Staff speak knowledgably about the difference between supporting a person to perform an activity – either themselves or with support – and performing the activity on the person's behalf.
The person and their family talk about the skills they have learned and the things they are learning now.
What to look for in documentation
Evidence of activity scripts, or similar, which set out the exact process and steps involved in teaching someone a specific skill. The scripts also maintain consistency between different staff members teaching the skill.
Support plans and skill-teaching programmes include targets that build on skills the person already has.
Red flags:
- Skills teaching is only given once a week - or very rarely. There is no evidence of continuous learning or skills teaching conducted by staff.
- Instead of teaching a skill, staff are performing the task for the person. For example, making an omelette rather than teaching the person to make the omelette.
- Staff are inconsistent in how they teach specific skills, which means the person is less likely to learn the skill. This potentially results in frustration and behaviour that challenges.
14. Do staff know the protocols for each person and their own role in the delivery of the support plan?
Key questions: caring, responsive, well-led
What might you see?
Staff confidently support the person through a teaching target, an assessment or a strategy for managing behaviour that challenges according to the person's support plan.
Consistency in the delivery of support for each person across all members of staff.
What might you hear?
Staff explain their role as set out in the programme, without needing to refer to the written documentation. Their explanation of their role must match what you are seeing in the service.
Staff speak knowledgeably and confidently about the protocols for responding to behaviours that challenge for each person. Their description should match the protocols noted in each person's behaviour support plan.
Staff talk about how important the activities and plans are for the person and what they mean to the person.
What to look for in documentation
Staff support roles are clearly set out in each person's support plan.
Red flags:
- Staff do not know their roles in each person's support plan or the person-specific protocols for addressing behaviours that challenge for each person.
- The support that a person receives differs from one member of staff to another. This includes strategies used to manage behaviours, teaching targets and the way that skills are taught.
Section 4: Is there a balance of programme components and are support plans for each person coherent across settings and over time?
It should be clear from observations, discussions, and documentation that the support plans achieve a good balance in terms of content, time and in relation to other programmes (ref PBS Competence Framework 'Developing and Implementing a Behaviour Support Plan (BSP)').
15. Is there a balance across multiple programmes, if relevant?
Key questions: caring, responsive
What might you see?
Evidence in the person's daily activities and their support that the needs outlined in their support plans are being met in proportion to the domains the plans address.
Evidence that people's activities fit with their wishes and longer-term aspirations, and that they promote quality of life.
What might you hear?
Staff are aware there can be multiple programmes being developed for people. They speak about how these programmes line up with one another.
What to look for in documentation
Support plans for each person match up with other programmes that have been developed for them. For example, the communication needs mentioned in the behaviour support plan match with those in the speech and language therapist plan.
In each person's programme there is advice or methods for promoting belonging. This includes access to the community, people, places, and things the person is interested in doing.
Programmes and behaviour support plans for each person line up with information provided by medical officials. For example, side effects for any medication the person may be taking.
Red flags:
- Daily activities for each person do not match up with the programmes for that person.
- A disproportionate amount of time is focused on just one or two aspects of the support outlined for the person. For example, spending more time on occupational therapy exercises than skills building.
16. Is the support provided to the person seamless across services and between professionals involved in the person's life?
Key questions: caring, responsive
What might you see?
Evidence that all service staff and relevant professionals are working within a positive behaviour support framework.
Characteristics of support - such as offering choice and being kind, nurturing and respectful - are demonstrated by all service staff and relevant professionals.
All staff and professionals working with each person offer the same high-quality level of support so that support for each person is consistent and always at its best. For instance, people should receive the same quality of support from their primary support staff as they do from their occupational therapist.
There is no change in the quality of support - it's kept at a high level - as people transition from one activity to another. This includes where there's a change of staff.
What might you hear?
All staff and professionals speak knowledgably about each person, with a clear commitment to keeping their quality of support consistent and at a high level.
Staff speak knowledgably about the support provided by professionals working with the person.
People and their families talk positively about the support they are getting across all aspects of the service provided.
What to look for in documentation
Evidence that multi-disciplinary assessments link up with one another. For example, recognition of medical needs for each person in a behaviour support plan.
Red flags:
- Difference in the quality of support provided by the service, staff and professionals.
- Support is organised around the service's needs, rather than the person's. For example, arranging rotas in a way most convenient for staff or offering activities based on staff availability.
17. Does each person's plan reflect planning for the future and a progression towards longer-term aspirations, as well as providing continuity over their life journey?
Key questions: caring, responsive
What might you see?
The service changes people's programmes, with help from all stakeholders, as the people themselves change.
Evidence that, over time, people's support takes account of changes in what they like and want, and their skills.
Daily routines include activities and learning that build skills people need to meet longer-term goals.
What might you hear?
Staff speak about the life history and life development of each person, with an idea of how that person would like their lifespan to unfold.
People and their family talk optimistically about the future and the goals they are working towards.
What to look for in documentation
Evidence of end goals in each person's programme. The goals are things they want and that have been agreed by all stakeholders, including the person themselves where possible. For example, living in the community, or in a shared residential house.
Red flags:
- No evidence or consideration of the person's aspirations or end goals.
- The person's support plans show little or no continuity across their lifespan.